A Toxic Side Effect of the Coronavirus: Financial Unwellness
One in two people in the U.S. say their financial health has been negatively impacted by the COVID-19 pandemic, through job loss, income disruption, or reduced work hours. The 2020 Financial Wellness Census, from Prudential found that one-half of U.S. adults are anxious about their financial future as of May 2020, an increase from 38% in late 2019. Prudential surveyed 3,000 U.S. adults across three generational cohorts: Millennials, Gen X, and Baby Boomers. The economic hit from the pandemic has disproportionately impacted people of color, younger people, women, small business owners, gig workers, and people working in retailer harder than
From Dr. Fauci to Peloton, Healthcare and Wellness Baked Into Ad Age’s Top 20 Brands for 2020
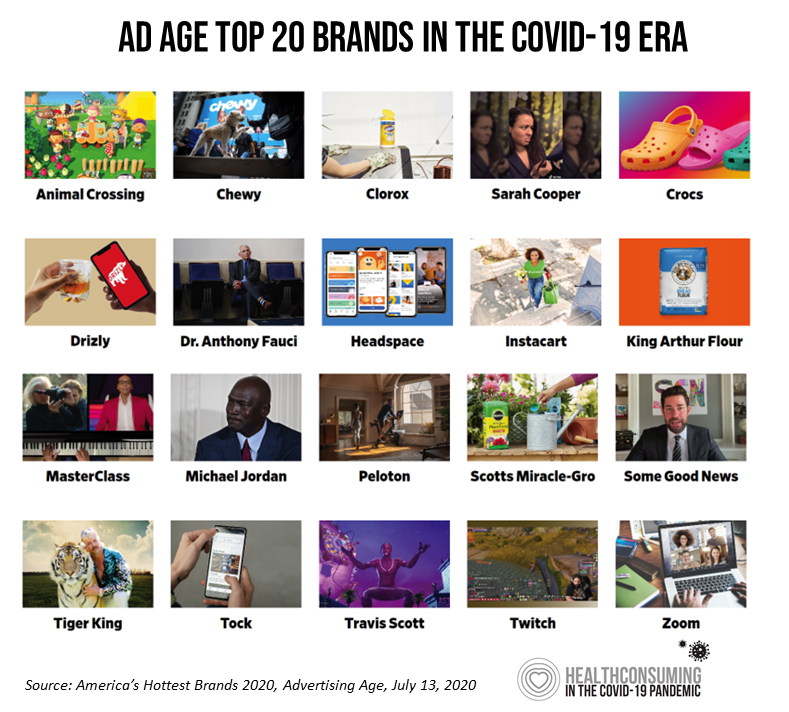
Advertising Age announced their list of the top 20 brands in 2020 this week. Ad Age’s lens on these was heavily tinted by consumers’ lives coping with the coronavirus pandemic: “The coronavirus has brought new attention to typically boring, decades-old consumer staples, while hastening the rise of digital newcomers that were only just beginning to gain traction pre-pandemic,” Ad Age explains in the introduction to the list of the selected brands. As the editors of the MadMen-and-Women’s most influential industry publication, they explain, “Ad Age chronicles 20 brands that are having a moment.” This moment to them as well as
How Can Healthcare Bring Patients Back? A Preview of Our ATA Session, “Onward Together” in the COVID Era

Today kicks off the first all-virtual conference of the ATA, the American Telemedicine Association. ATA’s CEO Ann Mond Johnson and team turned on a dime over the past few months, migrating the already-planned live conference scheduled in early May to this week, all online. I’ll be midwifing a panel this afternoon at 440 pm Eastern time, initially focused on how health care can garner patient loyalty. That theme was given to us in the fourth quarter of 2019, when initial planning for ATA 2020 had begun. What a difference a few months make. Not only has ATA pivoted to an
Juneteenth 2020: Inequality and Injustice in Health Care in America
“Of all the forms of inequality, injustice in health is the most shocking and the most inhuman because it often results in physical death,” Martin Luther King, Jr., asserted at the second meeting of the Medical Committee for Human Rights in Chicago on March 25, 1966. This quote has been shortened over the five+ decades since Dr. King told this truth, to the short-hand, “Of all the forms of inequality, injustice in health care is the most shocking and inhumane.” Professor Charlene Galarneau recently enlightened me on Dr. King’s original statement in her seminal essay, “Getting King’s Words Right.” Among
Economic Anxieties Rise, Medical and Vacation Plans Delayed: the COVID-19 Consumer in June 2020
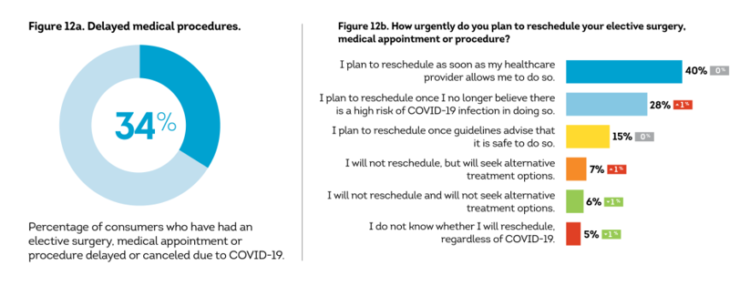
Some 6 in 10 people in the U.S. have been financially impacted by COVID-19. Those most negatively affected by the pandemic tend to be younger, Gen Z age group and African-American, 63% of whom felt financial pressure directly due from the virus and the national economic lockdown. By late May 2020, 34% of black Americans had lost their jobs compared with 21% in late April, compared with 18% of white consumers, reported in The COVID-19 Pandemic’s Financial Impact on U.S. Consumers, survey research from TransUnion. This post describes data from TransUnion’s Wave 9 report, which polled 2,086 U.S. adults 18
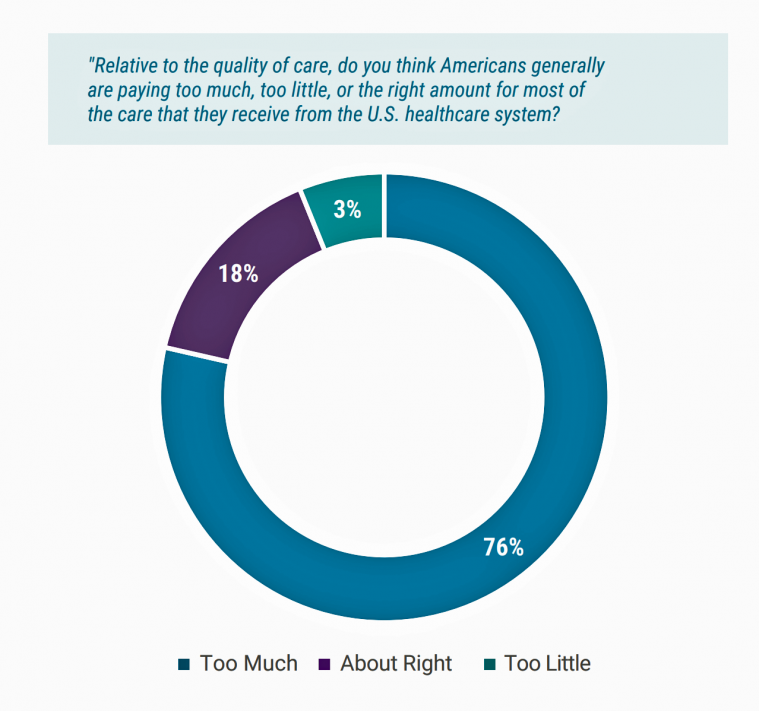
Americans’ Concerns About the US Healthcare System Loom Larger Than Worries About Their Own Care
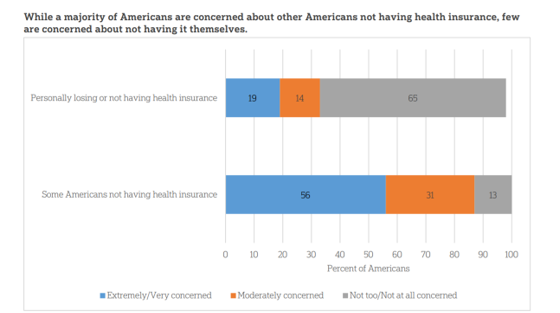
The coronavirus pandemic has further opened the kimono of the U.S. healthcare system to Americans: four months into the COVID-19 outbreak, most consumers (62%) of people in the U.S. are more concerned about other people not having access to high quality health care versus themselves. This is a 16 point increase in concern in May 2020 compared with the response to the same question asked in February in a poll conducted by the University of Chicago Harris School of Public Policy and The Associated Press-NORC Center for Public Affairs Research (the AP-NORC Center). The AP-NORC Poll found more of this
The Hair Economy in the COVID-19 Pandemic: Control, Wellness, and Self-Care

The barbershop and beauty salon are important community touch points for health, wellness, and social connection in so many peoples’ lives. In my book, HealthConsuming: From Health Consumer to Health Citizen, I feature the black barbershop to introduce a chapter on “The New Retail Health.” In the COVID-19 pandemic, how we’re dealing with hair is a metaphor for personal control, for political statements, for mental health, and for overall well-being. Check out Geoff Coates’ (known as Sadochicken, from Vancouver) take on “how quarantine hairdos are lookin’,” here. Can you see yourself? I can (it’s the “Corona Bangs” style for me,
Financial Insecurity Among U.S. Workers Will Worsen in the Pandemic — Especially for Women
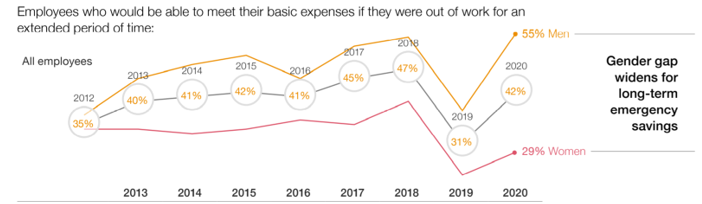
Millions of mainstream, Main Street Americans entered 2020 feeling income inequality and financial insecurity in the U.S. The coronavirus pandemic is exacerbating financial stress in America, hitting women especially hard, based on PwC’s 9th annual Employee Financial Wellness Survey COVID-19 Update. For this report, PwC polled 1,683 full-time employed adults between 18 and 75 years of age in January 2020. While the survey was conducted just as the pandemic began to emerge in the U.S., PwC believes, “the areas of concern back in January will only be more pronounced today,” reflecting, “the realities of the changing employee circumstances we are
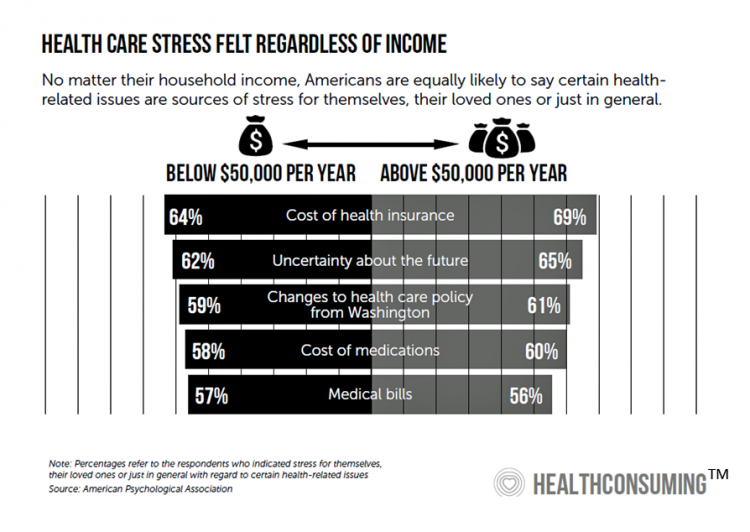
Stress in America – COVID-19 Takes Toll on Finances, Education, Basic Needs and Parenting

“The COVID-19 pandemic has altered every aspect of American life, from health and work to education and exercise,” the new Stress in America 2020 study from the American Psychological Association begins. The APA summarizes the impact of these mass changes on the nation: “The negative mental health effects of the coronavirus may be as serious as the physical health implications,” with COVID-19 stressors hitting all health citizens in the U.S. in different ways. Beyond the risk of contracting the virus, the Great Lockdown of the U.S. economy has stressed the U.S. worker and the national economy, with 7 in 10
How COVID-19 Is Driving More Deaths of Despair
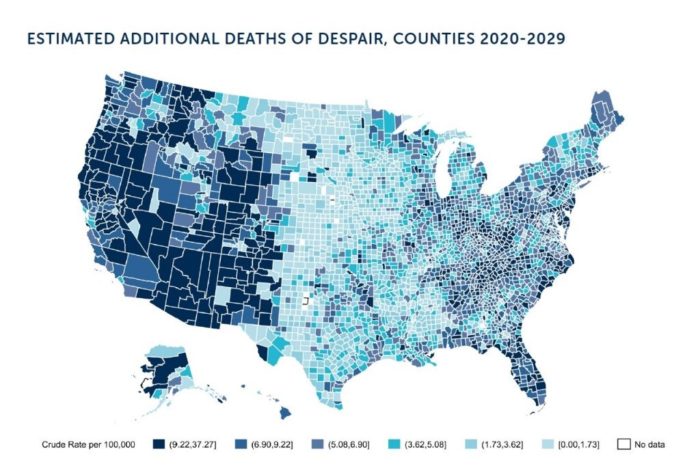
In the current state of the COVID-19 pandemic, we all feel like we are living in desperate times. If you are a person at-risk of dying a Death of Despair, you’re even more at-risk of doing so in the wake of the Coronavirus in America. Demonstrating this sad fact of U.S. life, the Well Being Trust and Robert Graham Center published Projected Deaths of Despair from COVID-19. The analysis quantifies the impact of isolation and loneliness combined with the dramatic economic downturn and mass unemployment with the worsening of mental illness and income inequity on the epidemic of Deaths of
How COVID-19 is Hurting Americans’ Home Economics in 2020
Beyond the physical and clinical aspects of the COVID-19 pandemic are financial hits that people are taking in the shutdown of large parts of the U.S. economy, impacting jobs, wages, and health insurance rolls. Some 1 in 2 people in the U.S. who have had their income impacted by the coronavirus have either fallen behind in paying off credit card debt or other bills, had problems paying for utilities, have lagged in paying for housing (rent or mortgage), been challenged paying for food, or other out-of-pocket costs. We learn about these fiscal hits from COVID-10 from the latest Health Tracking Poll
Health, Wealth & COVID-19 – My Conversation with Jeanne Pinder & Carium, in Charts
The coronavirus pandemic is dramatically impacting and re-shaping our health and wealth, simultaneously. Today, I’ll be brainstorming this convergence in a “collaborative health conversation” hosted by Carium’s Health IRL series. Here’s a link to the event. Jeanne founded ClearHealthCosts nearly ten years ago, having worked as a journalist with the New York Times and other media. She began to build a network of other journalists, each a node in a network to crowdsource readers’-patients’ medical bills in local markets. Jeanne started in the NYC metro and expanded, one node at a time and through many sources of funding from not-for-profits/foundations,
In the U.S., the Spread of Infectious Disease Now Seen As Bigger Threat Than Terrorism – Pew
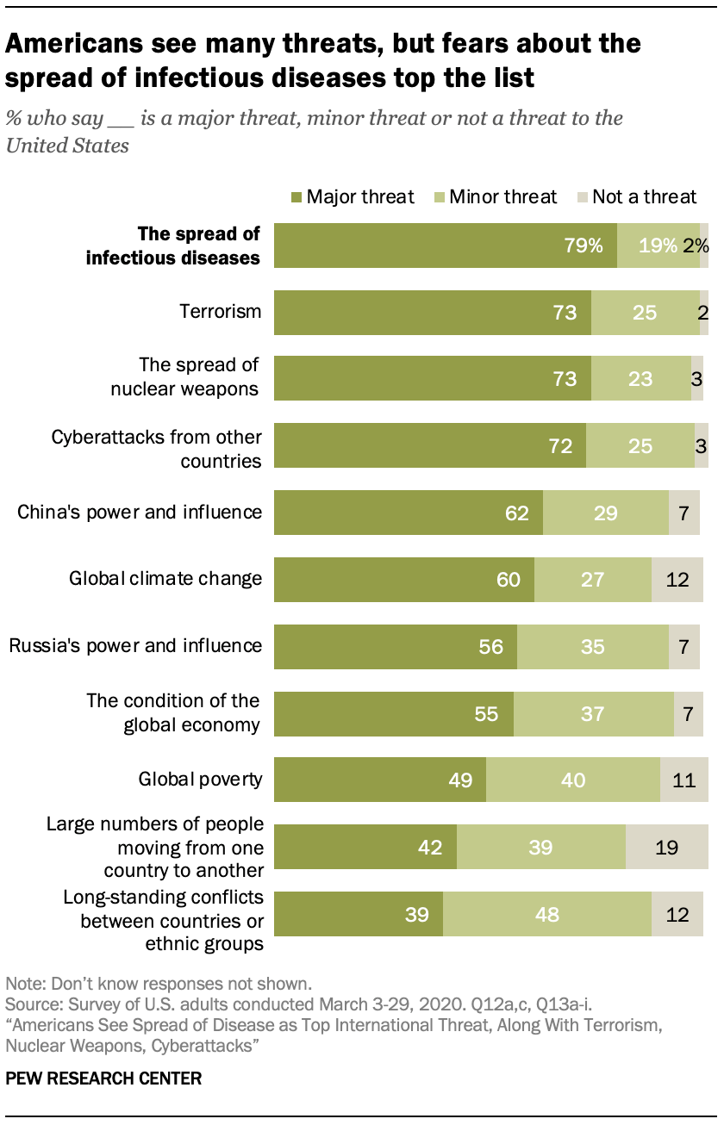
The spread of infectious disease is the new terrorism in the eyes of Americans. The most significant major threat to the U.S. is infectious disease, four in five Americans said in March 2020, closely followed by terrorism (in general), the spread of nuclear weapons, and cyberattacks from other countries. For the study, the Pew Research Center commissioned a telephone survey conducted among 1,000 U.S. adults in March 2020. Large majorities of people are also highly concerned about China’s growing power and influence, global climate change, Russia’s power and influence, the condition of the global economy, and global poverty. The percent
The Coronavirus Impact on American Life, Part 2 – Our Mental Health
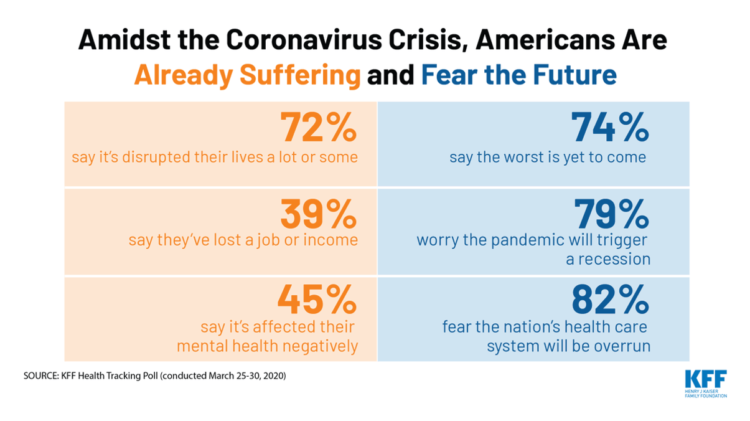
As the coronavirus pandemic’s curve of infected Americans ratchets up in the U.S., people are seeking comfort from listening to Dolly Parton’s bedtime stories, crushing on Dr. Anthony Fauci’s science-wrapped-with-empathy, and streaming the Tiger King on Netflix. These and other self-care tactics are taking hold in the U.S. as most people are “social distancing” or sheltering in place, based on numbers from the early April 2020 Kaiser Family Foundation health tracking poll on the impact of the coronavirus on American life. While the collective practice of #StayHome to #FlattenTheCurve is the best-practice advice from the science leaders at CDC, the NIAID
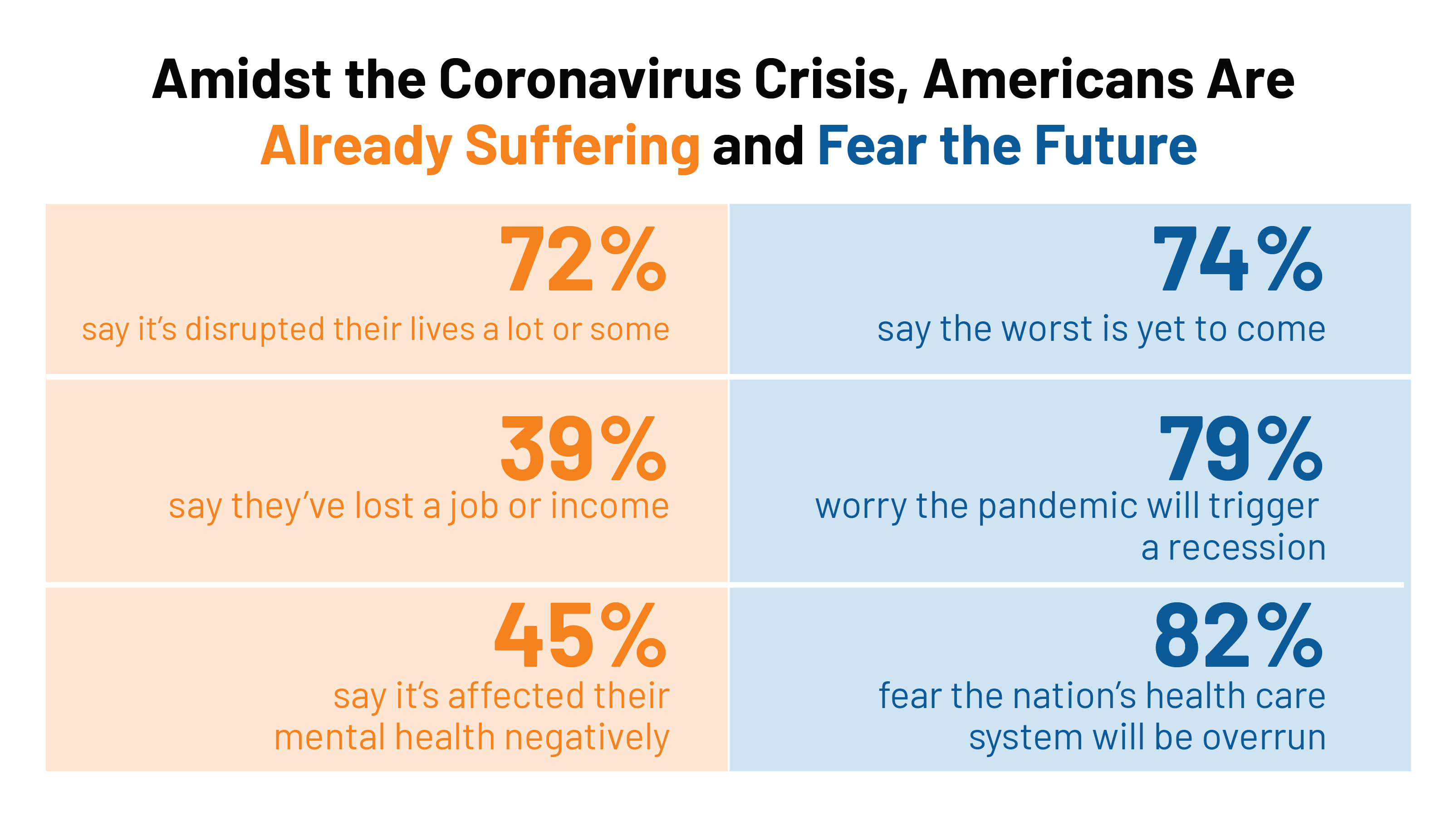
The Coronavirus Impact on American Life, Part 1 – Life Disrupted, and Money Concerns
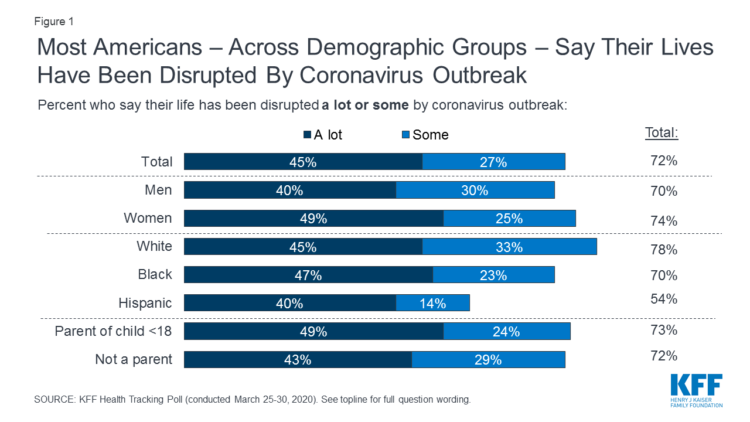
Nearly 3 in 4 Americans see their lives disrupted by the coronavirus pandemic, according to the early April Kaiser Family Foundation Health Tracking Poll. This feeling holds true across most demographic factors: among both parents and people without children; men and women alike; white folks as well as people of color (although fewer people identifying as Hispanic, still a majority). There are partisan differences, however, in terms of who perceives a life-disruption due to COVID-19: 76% of Democrats believe this, 72% of Independents, and 70% of Republicans. Interestingly, only 30% of Republicans felt this way in March 2020, more than
Wistful Thinking: The National Health Spending Forecast In a Land Without COVID-19
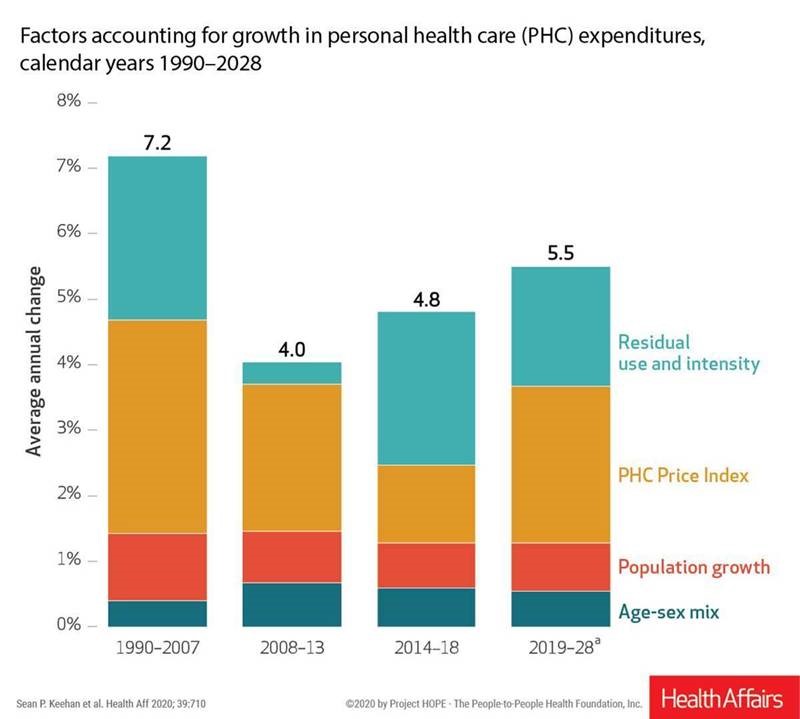
U.S. health care spending will grow to 20% of the national economy by 2028, forecasted in projections pre-published in the April 2020 issue of Health Affairs, National Health Expenditure (NHE) Projections. 2019-28: Expected Rebound in Prices Drives Rising Spending Growth. NHE will grow 5.4% in the decade, the model expects. But…what a difference a pandemic could make on this forecast. This year, NHE will be $3.8 trillion, growing to $6.2 trillion in 2028. Hospital care spending, the largest single component in national health spending, is estimated at $1.3 trillion in 2020. These projections are based on “current law,” the team
In the US COVID-19 Pandemic, A Tension Between the Fiscal and the Physical

“Act fast and do whatever it takes,” insists the second half of the title of a new eBook with contributions from forty leading economists from around the world. The first half of the title is, Mitigating the COVID Economic Crisis. The book is discussed in a World Economic Forum essay discussing the economists’ consensus to “act fast.” As the U.S. curve adds new American patients testing positive for the coronavirus, the book and essay illustrate the tension between health consumer versus the health citizen in the U.S. For clinical context, as I write this post on 24th March 2020, today’s U.S.
The COVID19 Consumer: #AloneTogether and More Health Aware
The number of diagnoses of people testing positive with the coronavirus topped 14,000 today in the U.S., Johns Hopkins COVID-19 interactive map told us this morning. As tests have begun to come on stream from California on the west coast to New York state on the east, the U.S. COVID-19 positives will continue to ratchet up for weeks to come, based on the latest perspectives shared by the most-trusted expert in America, Dr. Anthony Fauci. This report from the U.S. Department of Health and Human Services on the nation’s response to the coronavirus pandemic, published March 13, 2020, forecasts a
Estimates of COVID-19 Medical Costs in the US: $20K for inpatient stay, $1300 OOP costs
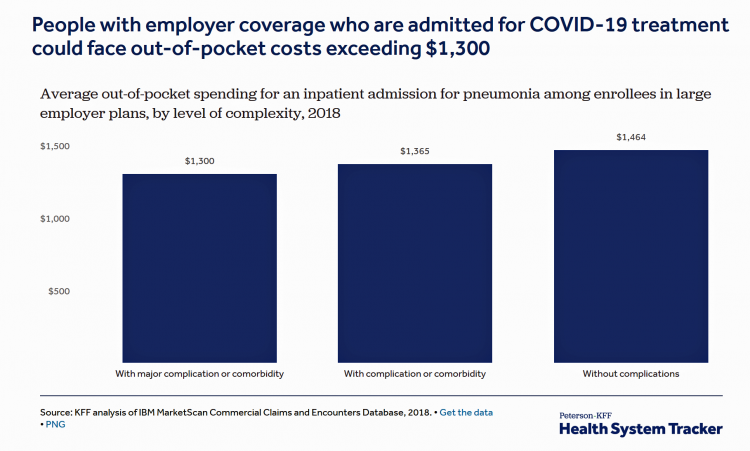
In the midst of growing inpatient admissions and test results for COVID-19, Congress is working as I write this post to finalize a round of legislation to help Americans with the costs-of-living and (hopefully) health care in a national, mandated, clarifying way. Right now in the real world, real patients are already being treated for COVID-19 in American hospitals. Patients are facing health care costs that may result in multi-thousand dollar bills at discharge (or death) that will decimate households’ financial health, particularly among people who don’t have health insurance coverage, covered by skinny or under-benefited plans, and/or lack banked
Waking Up a Health Consumer in the COVID-19 Era
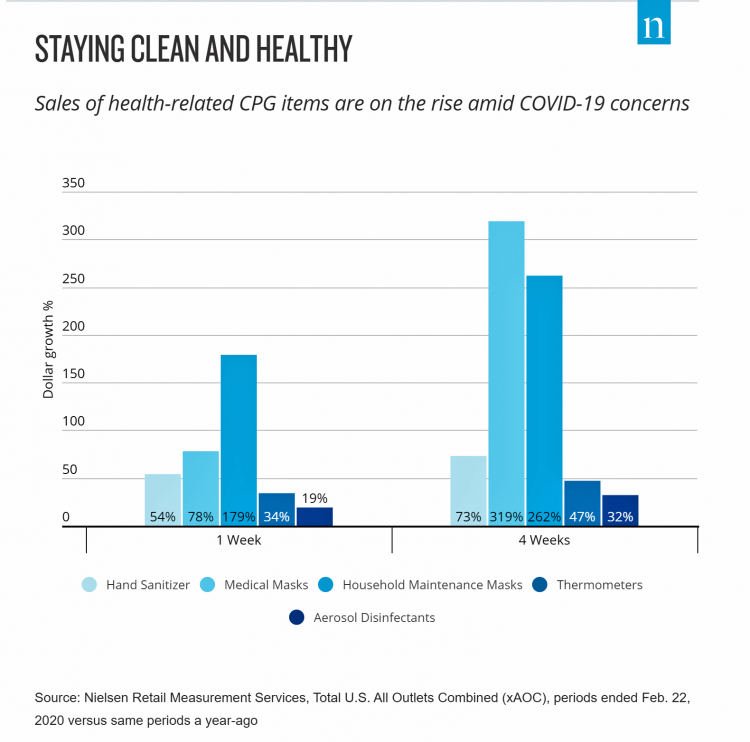
With President Trump’s somber speech from the Oval Office last night, we wake up on 12th March 2020 to a ban on most travel from Europe to the U.S., recommendations for hygiene, and call to come together in America. His remarks focused largely on an immigration and travel policy versus science, triaging, testing and treatment of the virus itself. Here is a link to the President’s full remarks from the White House website, presented at about 9 pm on 11 March 2020. Over the past week, I’ve culled several studies and resources to divine a profile of the U.S. consumer
The Book on Deaths of Despair – Deaton & Case On Education, Pain, Work and the Future of Capitalism
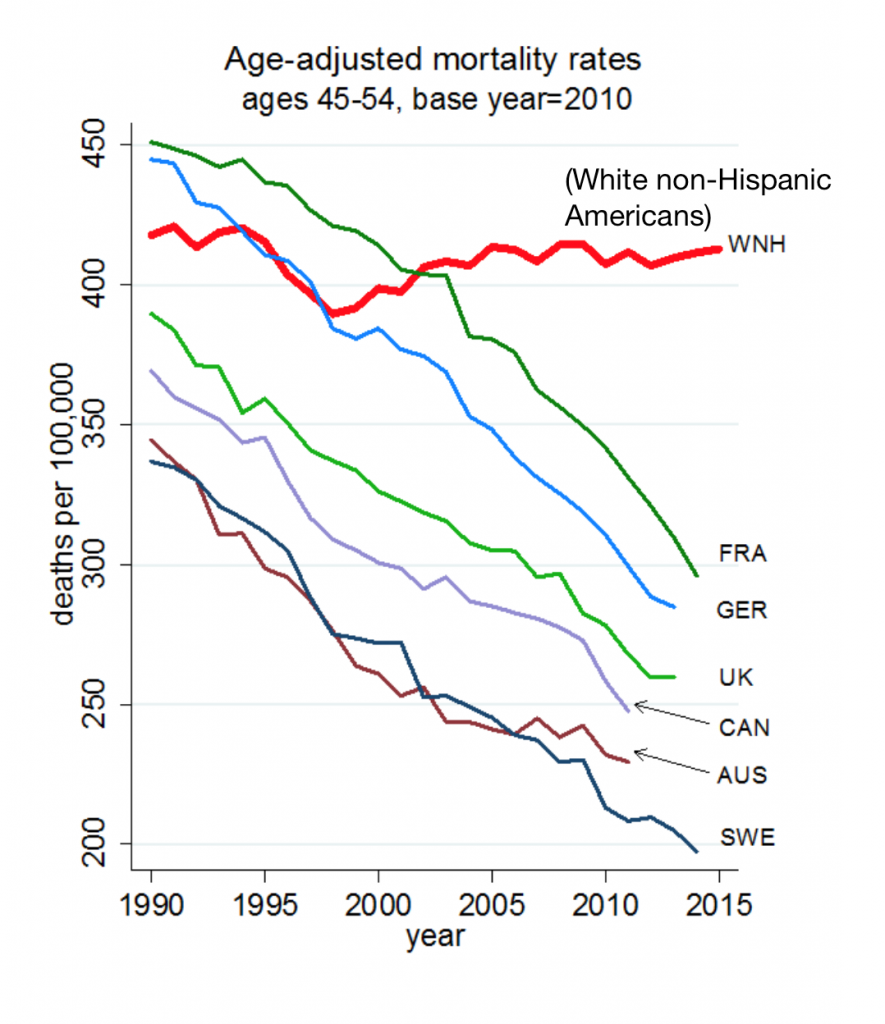
Anne Case and Angus Deaton were working in a cabin in Montana the summer of 2014. Upon analyzing mortality data from the U.S. Centers for Disease Control, they noticed that death rates were rising among middle-aged white people. “We must have hit a wrong key,” they note in the introduction of their book, Deaths of Despair and the Future of Capitalism. This reversal of life span in America ran counter to a decades-long trend of lower mortality in the U.S., a 20th century accomplishment, Case and Deaton recount. In the 300 pages that follow, the researchers deeply dive into and
“How’s Life?” for American Women? The New OECD Report Reveals Financial Gaps on International Women’s Day 2020
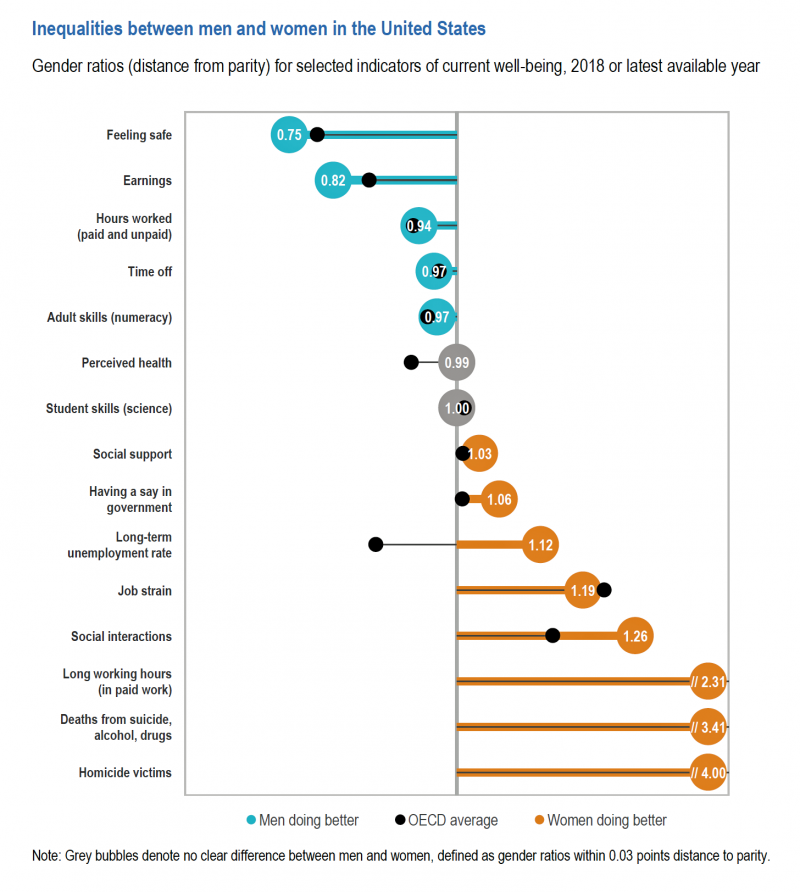
March 8 is International Women’s Day. In the U.S., there remain significant disparities between men and women, in particular related to financial well-being. The first chart comes from the new OECD “How’s Life?” report published today (March 9th) measuring well-being around the country members of the OECD. This chart focuses on women versus men in the United States based on over a dozen key indicators. Top-line, many fewer women feel safe in America, and earnings in dollars and hours worked fall short of men’s incomes. This translates into lower socioeconomic status for women, which diminishes overall health and well-being for
How Coronavirus Is Re-Shaping Consumer Behavior, From the Amusement Park to the Voting Booth

The coronavirus has shaken U.S. consumer confidence, both in terms of financial markets and personal health risks. COVID-19 is re-shaping peoples’ behavior and daily choices, from using public transit to choosing where to shop, based on Morning Consult’s National Tracking Poll #200276 conducted February 28-March 1, 2020. Morning Consult surveyed 2,200 U.S. adults, finding that 3 in 4 Americans were concerned about the coronavirus outbreak. The first chart from the survey shows various consumer activities by peoples’ likelihood of choosing to do them. Clearly, our daily life-flows outside of our homes have been impacted by our perceived risks of the coronavirus:
Job #1 for Next President: Reduce Health Care Costs – Commonwealth Fund & NBC News Poll

Four in five U.S. adults say lowering the cost of health care in America should be high priority for the next American president, according to a poll from The Commonwealth Fund and NBC News. Health care costs continue to be a top issue on American voters’ minds in this 2020 Presidential election year, this survey confirms. The first chart illustrates that lowering health care costs is a priority that crosses political parties. This is true for all flavors of health care costs, including health insurance deductibles and premiums, out-of-pocket costs for prescription drugs, and the cost of long-term care. While
The High Cost-of-Thriving and the Evolving Social Contract for Health Care
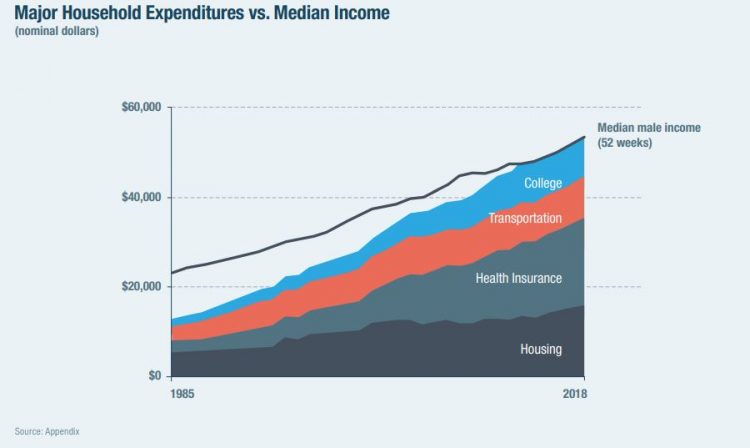
Millions of Americans have to work 53 weeks to cover a year’s worth of household expenses. Most Americans haven’t saved much for their retirement. Furthermore, the bullish macroeconomic outlook for the U.S. in early 2020 hasn’t translated into individual American’s optimism for their own family budgets. (Sidebar and caveat: yesterday was the fourth day in a row of the U.S. financial markets losing as much as 10% of market cap, so the global economic outlook is being revised downward by the likes of Goldman Sachs, Vanguard, and Morningstar, among other financial market prognosticators. MarketWatch called this week the worst market
Outpatient is the New Inpatient – The Future of Hospitals in America
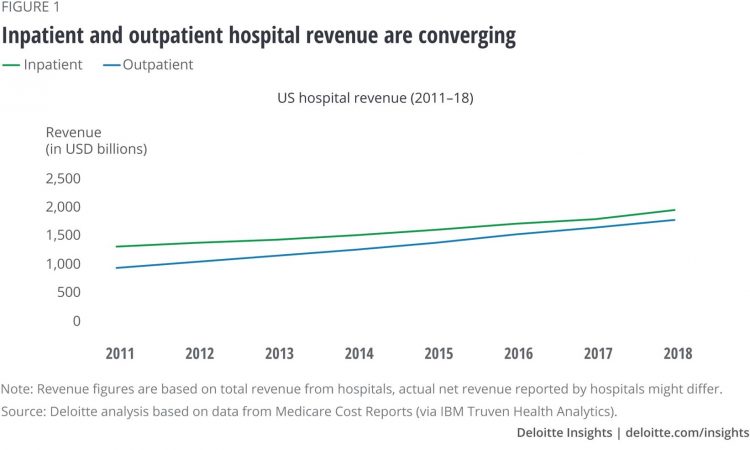
Outpatient revenue is crossing the curve of inpatient income. This is the new reality for U.S. hospitals and why I’ve titled this post, “outpatient is the new inpatient,” a future paradigm for U.S. hospitals This realization is informed by data in a new report from Deloitte, Where have the many hospital inpatient gone? The line chart illustrates Deloitte’s top and bottom line: “The shift toward outpatient is happening and will likely have a tremendous impact on operations, business models, staffing, and capital. Health systems should prepare for the future today and start thinking not only about how to manage their
Tools for Paying Medical Bills Don’t Help Health Consumers Manage Their Financial Health
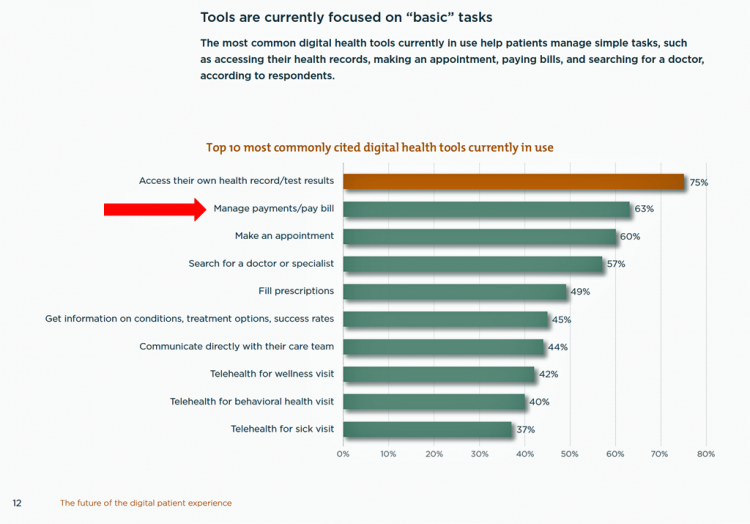
There’s a gap between the supply of digital health tools that hospitals and health systems offer patients, and what patients-as-consumers need for overall health and wellbeing. This chasm is illustrated in The future of the digital patient experience, the latest report from HIMSS and the Center for Connected Medicine (CCM). The big gap in supply to patients vs. demand by health consumers is highlighted by what the arrow in the chart below points to: managing payments and paying bills. Nowhere in the top 10 most commonly provided digital tools is one for price transparency, cost comparing or cost estimating. In the
Americans’ Top 2 Priorities for President Trump and Congress Are To Lower Health Care and Rx Costs
Health care pocketbook issues rank first and second place for Americans in these months leading up to the 2020 Presidential election, according to research from POLITICO and the Harvard Chan School of Public Health published on 19th February 2020. This poll underscores that whether Democrat or Republican, these are the top two domestic priorities among Americans above all other issues polled including immigration, trade agreements, infrastructure and regulations. The point that Robert Blendon, Harvard’s long-time health care pollster, notes is that, “Even among Democrats, the top issues…(are) not the big system reform debates…They’re worried about their own lives, their own
Most Workers and their Employers Want to Receive Digital Healthcare On-Demand
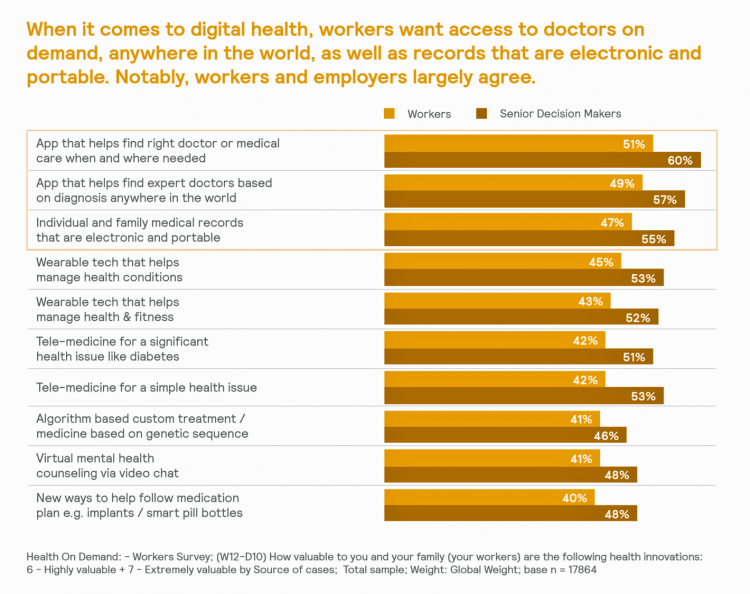
Most employers and their workers see the benefits of digital health in helping make health care more accessible and lower-cost, according to survey research published in Health on Demand from Mercer Marsh Benefits. Interestingly, more workers living in developing countries are keener on going digital for health than people working in wealthier nations. Mercer’s study was global, analyzing companies and their employees in both mature and growth economies around the world. In total, Mercer interviewed 16,564 workers and 1,300 senior decision makers in companies. The U.S. sample size was 2,051 employees and 100 decision makers. There’s a treasure trove of insights
The Federal Reserve Chairman Speaks Out on Health Care Costs: “Spending But Getting Nothing”
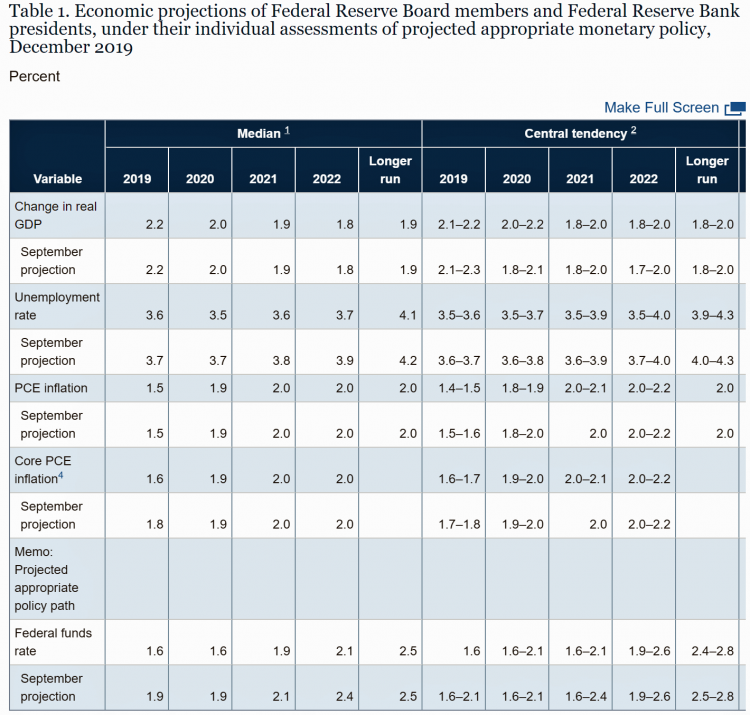
On February 12, 2020, the Chairman of the Federal Reserve Bank of the U.S. submitted the Semiannual Monetary Policy Report to Congress and testified to the Senate Banking Committee. Chairman Jerome Powell detailed the current state of the economy, discussing the state of the macroeconomy, GDP growth, unemployment, inflation, and projections for 2022 and beyond. The top line data points are shown in the first chart. After his prepared remarks, Chairman Powell responded to questions from members of the Senate Banking Committee. Senator Ben Sasse (R-Neb.) asked him about health care costs’ impact on the national U.S. economy. The Chairman
Health Care Costs Concern Americans Approaching Retirement – Especially Women and Sicker People
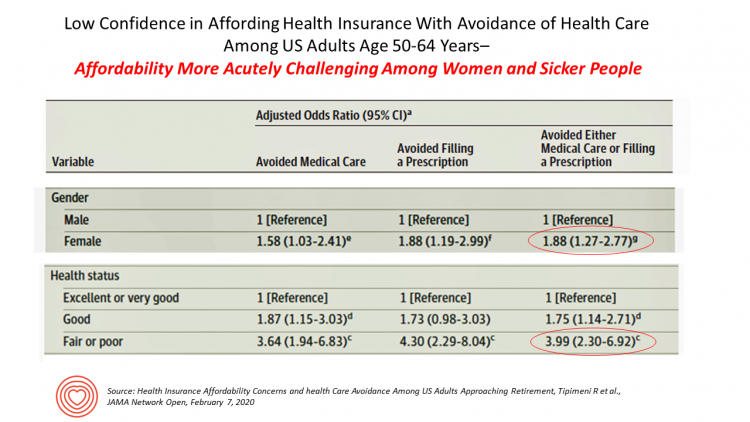
Even with the prospect of enrolling in Medicare sooner in a year or two or three, Americans approaching retirement are growing concerned about health care costs, according to a study in JAMA Network Open. The paper, Health Insurance Affordability Concerns and health Care Avoidance Among US Adults Approaching Retirement, explored the perspectives of 1,028 US adults between 50 and 64 years of age between November 2018 and March 2019. The patient survey asked one question addressing two aspects of “health care confidence:” “Please rate your confidence with the following:” Being able to afford the cost of your health insurance nad
A Uniting Issue in the United States is Lowering Prescription Drug Costs
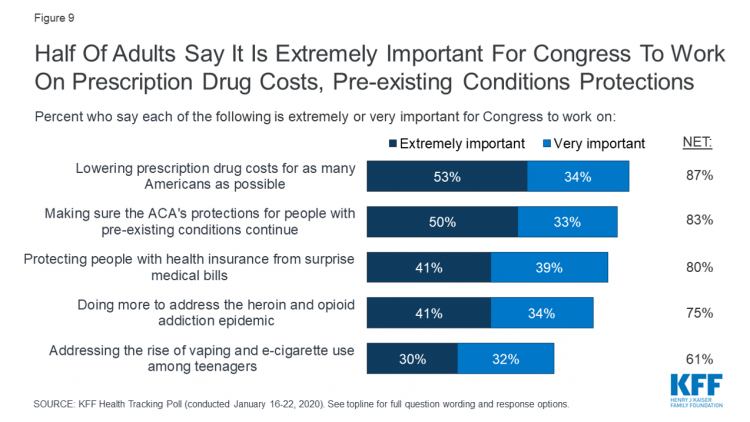
Health care continues to be the top-ranked voting issue in the U.S. looking to the November 2020 Presidential and Congressional elections. The Kaiser Family Foundation conducts the monthly poll which gauges U.S. adults’ perspectives on health care, and this month’s January 2020 Kaiser Health Tracking Poll explores Americans’ views on broad healthcare reform plans and specific medical policy issues. Overall, Americans point to prescription drug costs and the preservation of the Affordable Care Act’s protections for people with pre-existing conditions, the first chart tells us. Third and fourth on voters’ minds are protecting patients from surprise medical bills and better
Most Americans Regardless of Income Say It’s Unfair for Wealthier People to Get Better Health Care
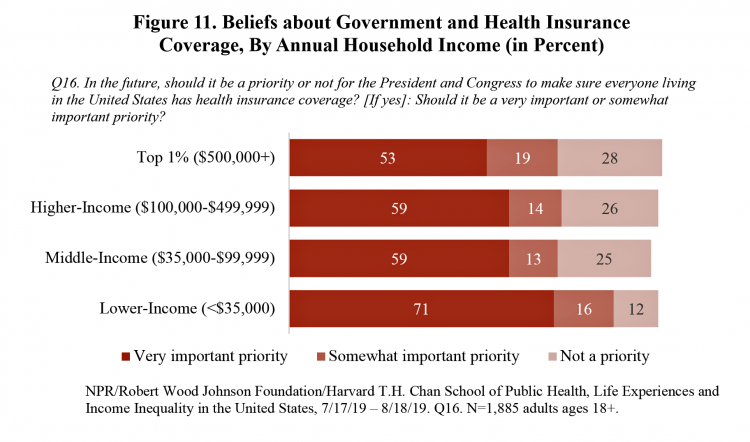
In America, earning lower or middle incomes is a risk factor for having trouble accessing health care and/or paying for it. But most Americans, rich or not, believe that it’s unfair for wealthier people to get better health care, according to a January 2020 poll from NPR, the Robert Wood Johnson Foundation and Harvard Chan School of Public Health, Life Experiences and Income Equality in the United States. The survey was conducted in July and August 2019 among 1,885 U.S. adults 18 or older. Throughout the study, note the four annual household income categories gauged in the research: Top 1%
Income Inequality is Fostering Mis-Trust, the Edelman 2020 Trust Barometer Observes
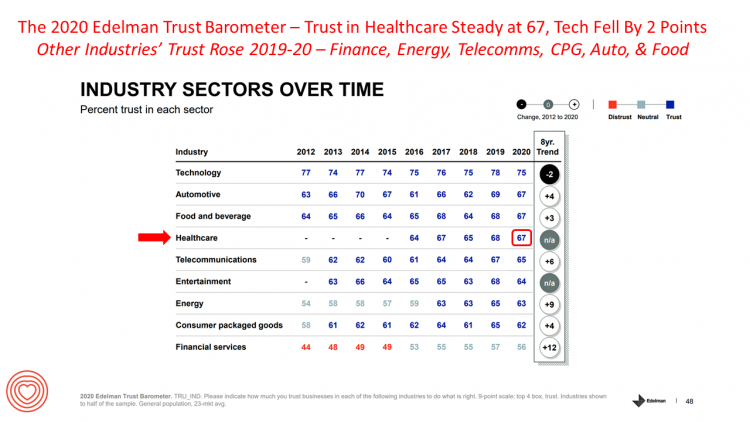
Economic development has historically built trust among nations’ citizens. But in developed, wealthier parts of the world, like the U.S., “a record number of countries are experiencing an all-time high ‘mass-class’ trust divide,” according to the 2020 Edelman Trust Barometer. For 20 years, Edelman has released its annual Trust Barometer every year at the World Economic Forum in Davos, recognizing the importance of trust in the global economy and society. Last year, it was the employer who was the most-trusted touch-point in citizens’ lives the world over, I discussed in Health Populi one year ago. This year, even our employers can’t
Consumers Seek Benefits From Food, a Personal Social Determinant of Health
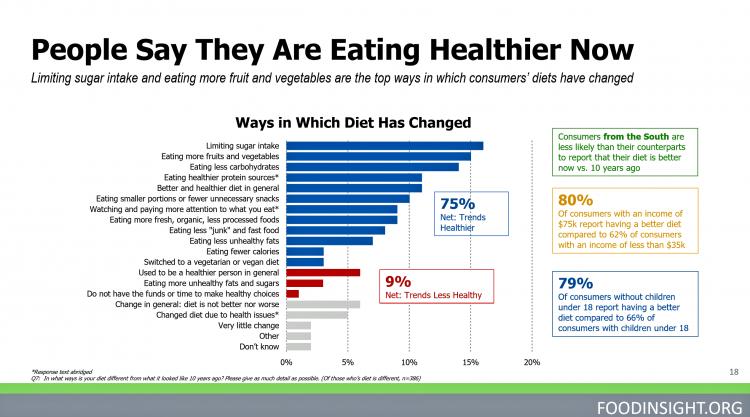
As consumers in the U.S. wrestle with accessing and paying for medical benefits, there’s another sort of health benefit people increasingly understand, embrace, and consume: food-as-medicine. More people are taking on the role of health consumers as they spend more out-of-pocket on medical care and insurance, and seeking food to bolster their health is part of this behavior change. One in four Americans seek health benefits from food, those who don’t still seek the opportunity to use food for weight loss goals, heart health and energy boosting, according to the 2019 Food & Health Survey from the International Food Information
Living in Digital Healthcare Times – Kicking off #DigitalHealthCES & #CES2020

Today is Day 1 of two Media Days at #CES2020 in Las Vegas, kicking off this manic week of the Consumer Electronics Show at the Mandalay Bay convention center. For several years, I’ve convened with journalists and industry analysts from around the world for these two days before the “official” opening of CES to hear the latest news from some of the largest tech-focused companies on Earth. Announcements come from across industry sector — from automotive and transportation, telecoms, consumer goods, entertainment, social media, travel, and retail…with platform technologies playing a role including but not limited to AI, AR/VR/XR (the
The 2020 Social Determinants of Health: Connectivity, Art, Air and Love
Across the U.S., the health/care ecosystem warmly embraced social determinants of health as a concept in 2019. A few of the mainstreaming-of-SDoH signposts in 2019 were: Cigna studying and focusing in on loneliness as a health and wellness risk factor Humana’s Bold Goal initiative targeting Medicare Advantage enrollees CVS building out an SDOH platform, collaborating with Unite US for the effort UPMC launching a social impact program focusing on SDoH, among other projects investing in social factors that bolster public health. As I pointed out in my 2020 Health Populi trendcast, the private sector is taking on more public health
In 2020, PwC Expects Consumers to Grow DIY Healthcare Muscles As Medical Prices Increase

The new year will see a “looming tsunami” of high prices in healthcare, regulation trumping health reform, more business deals reshaping the health/care industry landscape, and patients growing do-it-yourself care muscles, according to Top health industry issues of 2020: Will digital start to show an ROI from the PwC Health Research Institute. I’ve looked forward to reviewing this annual report for the past few years, and always learn something new from PwC’s team of researchers who reach out to experts spanning the industry. In this 14th year of the publication, PwC polled executives from payers, providers, and pharma/life science organizations. Internally,
Food As Medicine: Grocery Stores Expand as Health Destinations While the Federal Government Cuts Food Stamps
There’s something like cognitive dissonance as I prepare my 2020 Health Populi TrendCast of what to expect in the health/care ecosystem in the new year. One of my key pillars for health-making is food-as-medicine, and that opportunity in this moment resonates in this holiday season with Dickens’ “Best of Times, Worst of Times” context-setting that kicks off Great Expectations. In the “best of times” part of the food+health equation, we recognize the growing role of grocery stores, food-tech and food manufacturers in the health/care landscape. A current example comes from Kroger, partnering with Ascension’s health system in Tennessee, enhancing the organization’s
Hospitals Suffer Decline in Consumer Satisfaction

While customer satisfaction with health insurance plans slightly increased between 2018 and 2019, patient satisfaction with hospitals fell in all three settings where care is delivered — inpatient, outpatient, and the emergency room, according to the 2018-2019 ACSI Finance, Insurance and Health Care Report. ACSI polls about 300,000 U.S. consumers each year to gauge satisfaction with over 400 companies in 46 industries. For historic trends, you can check out my coverage of the 2014 version of this study here in Health Populi. The 2019 ACSI report bundles finance/banks, insurance (property/casualty, life and health) and hospitals together in one document. Health
Longevity Stalls Around the World And Wealth, More Concentrated

Two separate and new OECD reports, updating health and the global economic outlook, raise two issues that are inter-related: that gains in longevity are stalling, with chronic illnesses and mental ill health affecting more people; and, as wealth grows more concentrated among the wealthy, the economic outlook around most of the world is also slowing. First, we’ll mine the Health at a Glance 2019 annual report covering data on population health, health system performance, and medical spending across OECD countries. The first chart arrays the x-y data points of life expectancy versus health spending for each of the OECD countries
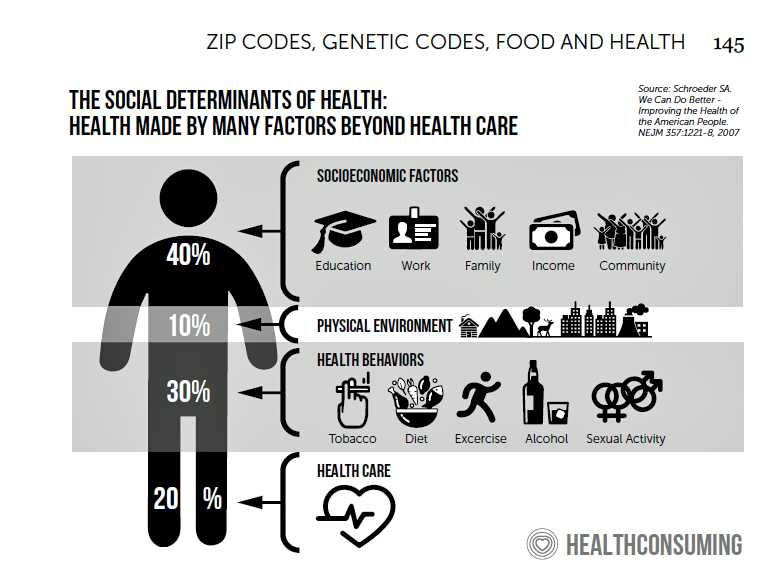
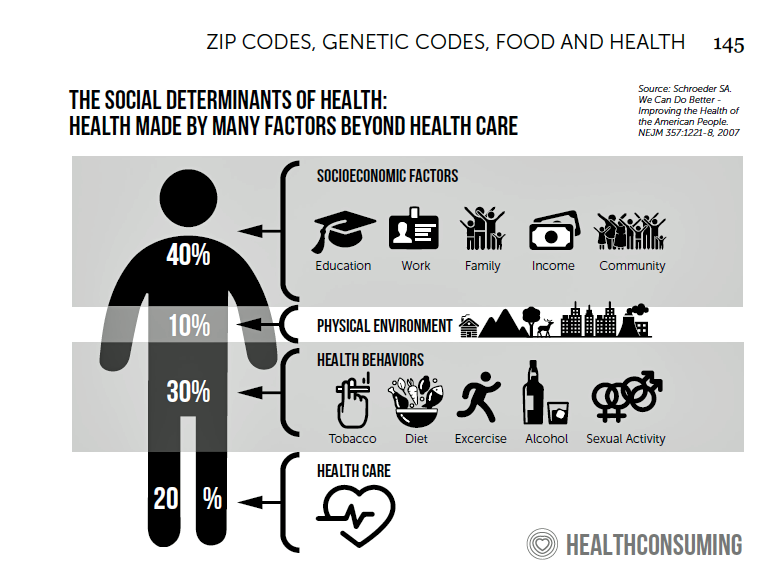
Social Determinants of Health – My Early Childhood Education and Recent Learnings, Shared at the HealthXL Global Gathering
My cousin Arlene got married in Detroit at the classic Book Cadillac Hotel on July 23, 1967, a Sunday afternoon wedding. When Daddy drove us back out to our suburban home about 30 minutes from the fancy hotel, the car radio was tuned to WWJ Newsradio 950, all news all the time. As soon as Daddy switched on the radio, we were shocked by the news of a riot breaking out in the city, fires and looting and gunshots and chaos in the Motor City. Two days later, my father, who did business with Mom-and-Pop retail store owners in the
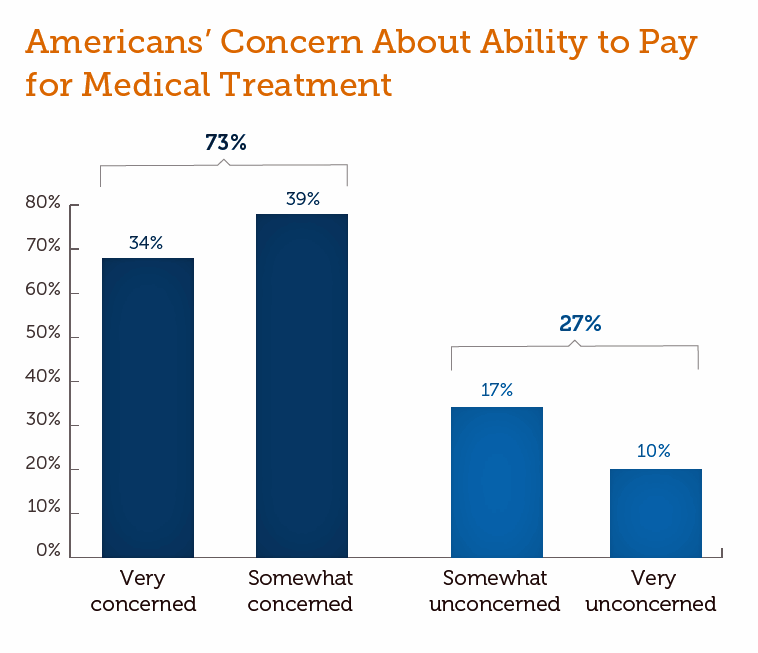
More Evidence of Self-Rationing as Patients Morph into Healthcare Payors

Several new studies reveal that more patients are feeling and living out their role as health care payors as medical spending vies with other household line items. This role of patient-as-the-payor crosses consumers’ ages and demographics, and is heating up health care as the top political issue for the 2020 elections at both Federal and State levels. In research from HealthPocket, 2 in 5 Americans said they needed to reduce other household expenses to be able to afford their monthly insurance premiums. Four in ten consumers said their monthly health insurance premiums were increasing. One in four people in the
A Tale of Two Americas as Told by the 2019 OECD Report on Health

It was the best of times, It was the worst of times, It was the age of wisdom, it was the age of foolishness, It was the epoch of belief, it was the epoch of incredulity, … starts Dickens’ Tale of Two Cities. That’s what came to my mind when reading the latest global health report from the OECD, Health at a Glance 2019, which compares the United States to other nations’ health care outcomes, risk factors, access metrics, and spending. Some trends are consistent across the wealthiest countries of the world, many sobering, such as: Life expectancy rates fell in 19 of the
The Link Between Wellness & Wealth Is Powerful for Everyone – and Especially Women

In the U.S., the link between wellness and wealth, money and health, is strong and common across people, young and old. But the impacts of money on health, well-being, and life choices varies across the ages, based on a study from Lively, a company that builds platforms for health savings accounts. The first chart illustrates that health care costs challenge people in many ways: the most obvious health care cost problems prevent people from saving more for retirement or paying down debt. Eight in 10 Americans concur that rising health care costs challenge their ability to save for retirement. Beyond the
Great Expectations for Health Care: Patients Look for Consumer Experience and Trust in Salesforce’s Latest Research

On the demand side of U.S. health care economics, patients are now payors as health consumers with more financial skin in paying medical bills. As consumers, people have great expectations from the organizations on the supply side of health care — providers (hospitals and doctors), health insurance plans, pharma and medical device companies. But as payors, health consumers face challenges in getting care, so great expectations are met with frustration and eroding trust with the system, according to the latest Connected Healthcare Consumer report from Salesforce published today as the company announced expansion of their health cloud capabilities. This is
Will Consumers Cross the Cost-and-Trust Chasm Between Prescription Drugs and Hospitals?
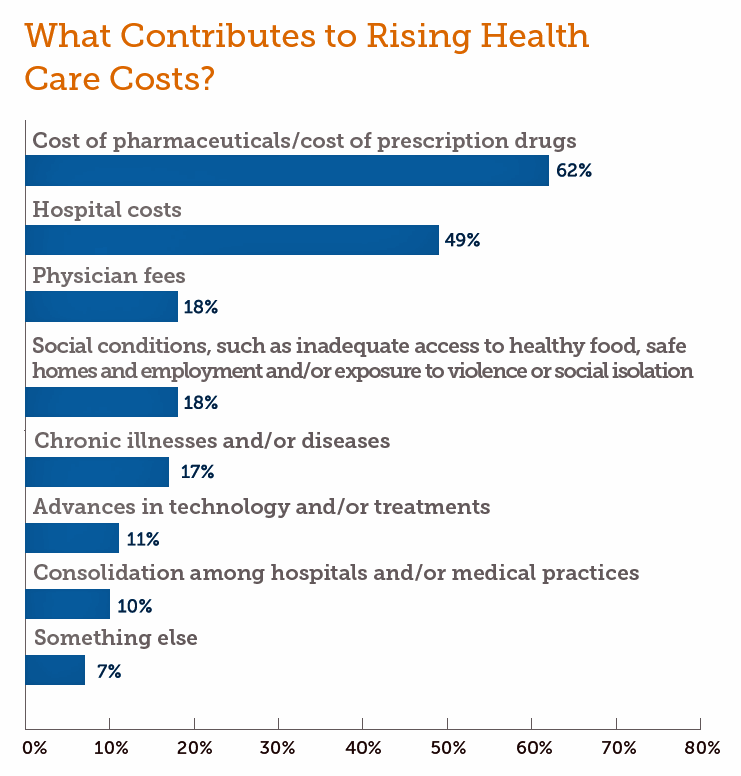
People in the U.S. rank prescription drugs, lab tests, emergency room visits, dental and vision care, preventive services, chronic disease management and mental health care as the “most essential” health care services, according to the 2019 Survey of America’s Patients conducted by The Physicians Foundation. When asked what factors contribute to rising health care costs in America, most consumers cite the cost of prescription drugs. Taken together, these two data points demonstrate the potent political import of prescription drug prices as the U.S. approaches the 2020 Presidential election. The Physicians Foundation surveyed 2,001 U.S. adults between 27 and 75 years
While Costs Are A Top Concern Among Most U.S. Patients, So Are Challenges of Poverty, Food, and Housing
Rising health care costs continue to concern most Americans, with one in two people believing they’re one sickness away from getting into financial trouble, according to the 2019 Survey of America’s Patients conducted for The Physicians Foundation. In addition to paying for “my” medical bills, most people in the U.S. also say that income inequality and inadequate social services significantly contribute to high medical spending for every health citizen in the nation. The Physicians Foundation conducts this study into Americans’ views on the U.S. health care system every other year. This year’s poll was conducted in September 2019 and included input
Americans’ Top Sources of Stress are Money, Money, Money and Family
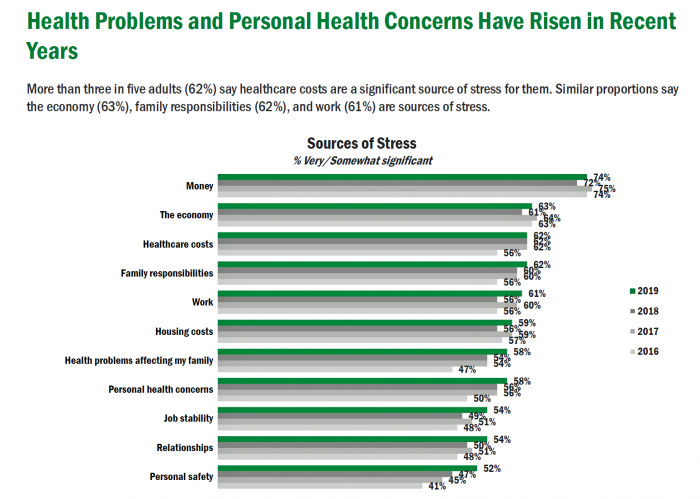
ABBA sang the song “Money Money Money” back in 1976. The lyrics feel, sadly, spot-on when thinking about health care costs, job-lock and Americans’ home economics in 2019. “Work all night, I work all day, to pay the bills I have to pay Ain’t it sad And still there never seems to be a single penny left for me That’s too bad… Money, money, money must be funny In the rich man’s world.” That year, ’76, wasn’t just the U.S. bicentennial — it was a year when the U.S. allocated 8.6% of the nation’s Gross Domestic Product for health care.
Patients Growing Health Consumer Muscles Expect Digital Services

Patients’ experiences with the health care industry fall short of their interactions with other industries — namely online retail, online banking and online travel, a new survey from Cedar, a payments company, learned. Survata conducted the study for Cedar among 1,607 online U.S. consumers age 18 and over in August and September 2019. These study respondents had also visited a doctor or hospital and paid a medical bill in the past year. One-third of these patients had a health care bill go to collections in the past year, according to Cedar’s 2019 U.S. Healthcare Consumer Experience Study. Among those people
The Hospital CFO in the Anxiety Economy – My Talk at Cerner’s Now/Next Conference
As patients have taken on more financial responsibility for first-dollar costs in high-deductible health plans and medical bills, hospitals and health care providers face growing fiscal pressures for late payments and bad debt. Those financial pressures are on both sides of the health care payment transaction, stressing patients-as-payors and health care financial managers alike. I’m speaking to health industry stakeholders on patients-as-payors at Cerner’s Now/Next conference today about the patient-as-payor, a person primed for engagement. That’s as in “Amazon-Primed,” which patients in their consumer lives now use as their retail experience benchmark. But consumers-as-patients don’t feel like health care today
The New Health/Care is Patient-Led, Retail-Enabled – The GMDC Self-Care Summit
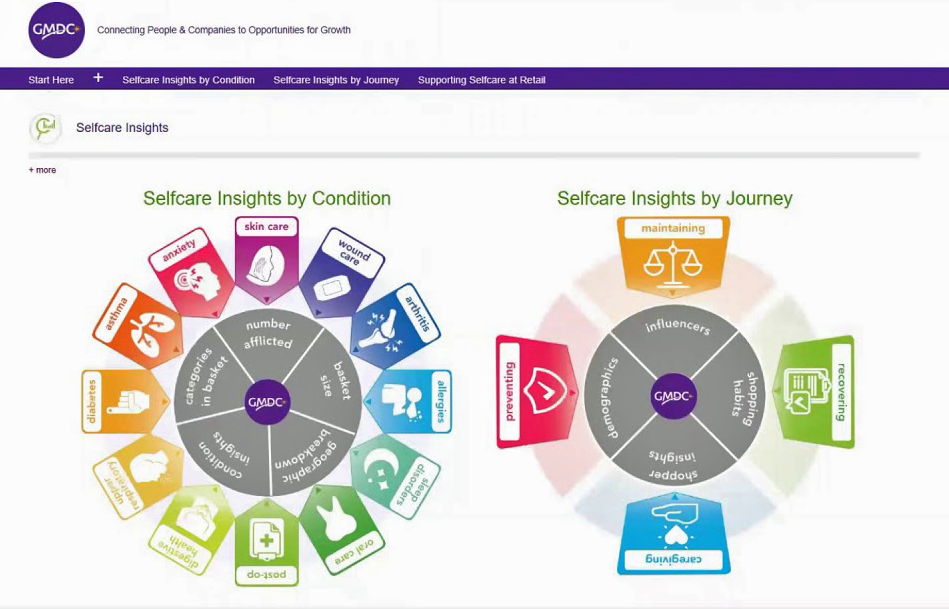
SelfCare is health/care, particularly as patients, everyday people, take on greater responsibility for clinical decisions and paying for medical services. We’re convening today through Sunday in Indianapolis with GMDC, the Global Market Development Center and Retail Tomorrow to brainstorm the current and future prospects for SelfCare, health and wellness in the hands, hearts, and homes of consumers. To bolster the message and engage with industry stakeholders, GMDC collaborated with the Hamacher Resource Group to develop a SelfCare Roadmap, an interactive tool that provides insights into twelve conditions where consumers typically looking to DIY their health using over-the-counter medicines, supplies and
Health @ Retail – Prelude to GMDC SelfCare Summit with Updates from Hims & Hers, GoodRx, Sam’s Club and Amazon Care
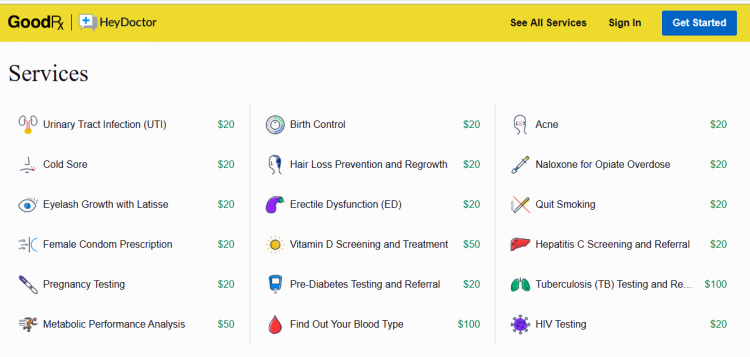
“We knew millions of people weren’t getting the care they needed — they were either too embarrassed to seek help or felt stuck in a system that was confusing and intimidating. Digital health has the potential to radically change the way people approach their wellness and, since launching in 2017, we’ve outpaced even our own expectations, delivering more than 1 million Hims & Hers products to our customers. In collaboration with highly-qualified doctors and healthcare providers, we’ve built a digital health platform that is changing the way people talk about and receive the care they need.” That’s a verbatim paragraph
The Rise of Social Determinants of Health in Healthcare is Just Real Life Stuff for People, Patients, Consumers

Based on the influx of research studies and position papers on social determinants of health flowing into my email box and Google Alerts, I can say we’re past the inflection point where SDoH is embraced by hospitals, professional societies, health plans and even a couple of pioneering pharma companies. PwC published a well-researched global-reaching report this week appropriately titled, Action required: The urgency of addressing social determinants of health. The “wheel of determinants” illustrates potential partners for collaborating in communities to address SDoH factors. The collaborators include governments, health care providers, payors, life science and pharma, tech and telecomms, policy
How Whirlpool’s #CareCounts Campaign Bolsters a Key Social Determinant of Health

Did you know that September is Attendance Awareness month? Me, neither. But reading one of last Sunday’s national newspapers, I noticed a full-page ad that read, “Whirlpool is helping keep kids in schools with washers and dryers.” Reading further on, the copy called out two data points making the point about laundry and education: One in five students don’t have access to clean clothes, making them more likely to miss school; and Students who miss school are 7 times more likely to drop out of educational system. The full ad’s theme in the words of Whirlpool is that, “Education has a
Talking “HealthConsuming” on the MM&M Podcast

Marc Iskowitz, Executive Editor of MM&M, warmly welcomed me to the Haymarket Media soundproof studio in New York City yesterday. We’d been trying to schedule meeting up to do a live podcast since February, and we finally got our mutual acts together on 6th August 2019. Here’s a link to the 30-minute conversation, where Marc combed through the over 500 endnotes from HealthConsuming‘s appendix to explore the patient as the new health care payor, the Amazon prime-ing of people, and prospects for social determinants of health to bolster medicines “beyond the pill.” https://www.pscp.tv/MMMnews/1eaJbvgovBYJX Thanks for listening — and if you
100 Million People in America Lack Broadband — an On-Ramp to Health and Safety

One in three Americans does not have a broadband connection, according to a new report from the NPD Group. This means that about 100 million people in the U.S. can’t benefit from telehealth and other digital health connections that can bolster self-care, home care, and lower cost care. Most of these folks in the broadband-digital divide live in rural America/ “The so-called digital divide, between those that can or cannot make the best use of the Internet, can be clearly felt in rural markets where the lack of broadband impacts everything from entertainment to the educational system,” Eddie Hold, President
On Amazon Prime Day, What Could Health Care Look Like?

Today is July 15, and my email in-box is flooded with all flavors of Amazon Prime’d stories in newsletters and product info from ecommerce sites — even those outside of Amazon from beauty retailers, electronics channels, and grocery stores. So I ask on what will probably be among the top ecommerce revenue generating days of all time: “What could health care look like when Amazon Prime’d?” I ask and answer this in my book, HealthConsuming, as chapter 3. For context, this chapter follows two that explain how patients in the U.S. have been morphing into health consumers based on how health
Gaps in Health Equity in America Are Growing

There’s been a “clear lack of progress on health equity during the past 25 years in the United States,” asserts a data-rich analysis of trends conducted by two professors/researchers from UCLA’s School of Public Health. The study was published this week in JAMA Network Open. The research mashed up several measures of health equity covering the 25 years from 1993 through 2017. The data came out of the Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System looking at trends by race/ethnicity, sex and income across three categories for U.S. adults between 18 and 64 years of age.
Prescription Drugs Are Becoming A Luxury Good in America – Join the #HCLDR Chat Tonight
“Drugmakers Push Their Prices Higher” is the top story under the Business & Finance banner in today’s Wall Street Journal. That’s in terms of drugs’ list prices, which most patients don’t pay. But drug costs to patients are in the eye of the beholder, who in a high-deductible plan or Medicare Part D donut hole becomes the first-dollar payer. Patients continue to face rising drug costs, pushing them into what I’ve been thinking about as luxury-goods territory. The economic definition of a luxury good is a product for which demand increases more than proportionally as income rises, so that spending
A Matter of Trust, Perception, Risk, and Uncertainty – The Big Issues Raised by the Acquisition of PatientsLikeMe and Other Patient Data Transactions

By Susannah Fox, Jane Sarasohn-Kahn and Lisa Suennen I’ve lived long enough to have learned The closer you get to the fire the more you get burned But that won’t happen to us Cause it’s always been a matter of trust A Matter of Trust, by Billy Joel If you’re in health care and don’t live under a rock, you have probably heard that United Health Group (UHG) has acquired PatientsLikeMe (PLM). After the announcement, there was a lot of sound and fury, some of which signified nothing, as the saying goes, and some which signified a lot.
Health Care and the Democratic Debates – Part 1 – Medicare For All, Rx Prices, Guns and Mental Health

Twenty Democratic Presidential candidates each have a handful of minutes to make their case for scoring the 2020 nomination, “debating” last night and tonight on major issues facing the United States. I watched every minute, iPad at the ready, taking detailed notes during the 120 minutes of political discourse conducted at breakneck speed. Lester Holt, Savannah Guthrie, and Jose Diaz-Balart asked the ten candidates questions covering guns, butter (the economy), immigration, climate change, and of course, health care — what I’m focusing on in this post, the first of two-debate-days-in-a-row. The first ten of twenty candidates in this debate were,
Kroger Health Thinks Food is Medicine – Nutrition at the Grocery Store Via FMI’s Insights
In reading the July/August issue of Eating Well magazine this week, I came across this ad which I scanned for you to see yourself: “We believe in food as medicine.” Signed, Kroger Health. Here’s the introductory text in the full-page ad: “As Kroger Health, our vision is to help people live healthier lives. And now, more than ever, through our experts, innovation, and technology, we’re uniquely positioned to bring that vision to life,” the copy read. “We know food,” the text continued, as part of The Kroger Co. which is the largest grocery chain in the U.S. celebrating 135 years
IKEA Garners the Top Health & Wellness Award at Cannes Lions 2019 – the Expanding Health/Care Ecosystem

“Health is now everyone’s business,” Shaheed Peera, Executive Creative Director of Publicis LifeBrands, said this week at the 2019 Cannes Lions awards. Shaheed also led the Health & Wellness jury at Cannes Lions 2019, the mission of which is to, in the words of the award’s portal, “celebrate creativity for personal wellbeing.” The Grand Prix Lions award for Health & Wellness went to IKEA for the company’s ThisAbles campaign. ThisAbles is a project pioneered by IKEA’s team in Israel, looking to improve everyday living for people with special needs through well-designed IKEA products. IKEA collaborated with non-profit organizations to develop
Americans Could Foster a Health Consumer Movement, Families USA Envisions
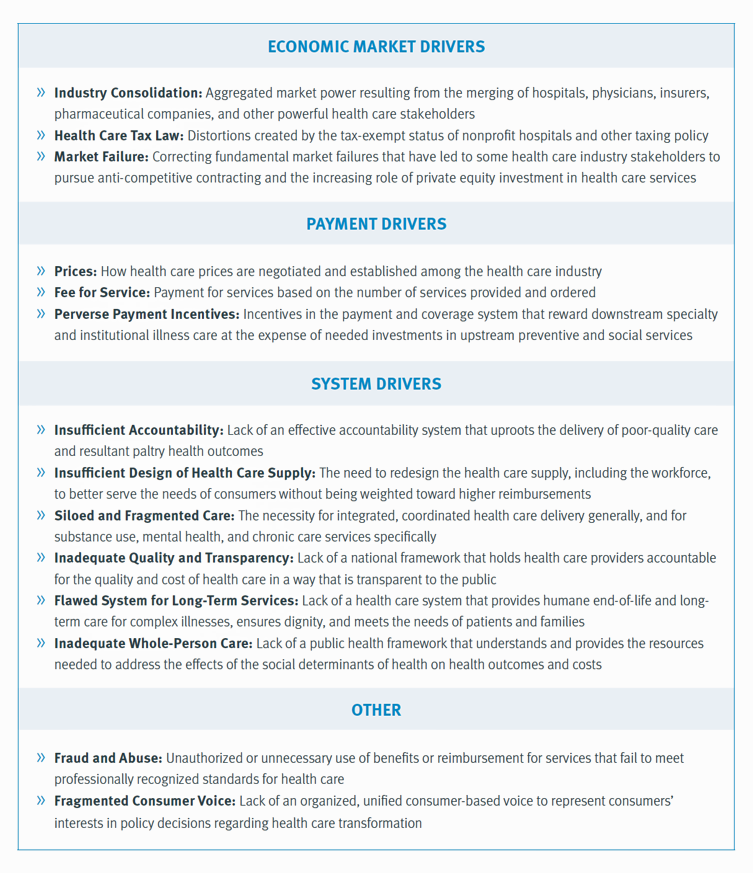
Employers, health care providers, unions, leaders and — first and foremost, consumers — must come together to build a more accessible, affordable health care system in America, proposes a call-to-action fostered by a Families USA coalition called Consumers First: The Alliance to Make the Health Care System Work for Everyone. The diverse partners in this Alliance include the American Academy of Family Physicians, AFSCME (the largest public service employees’ union in the U.S.), the American Benefits Council (which represents employers), the American Federation of Teachers (AFT), First Focus (a bipartisan children’s advocacy organization), and the Pacific Business Group on Health
People Want to Flourish, Not Just Live – Speaking Health Politics to Real People
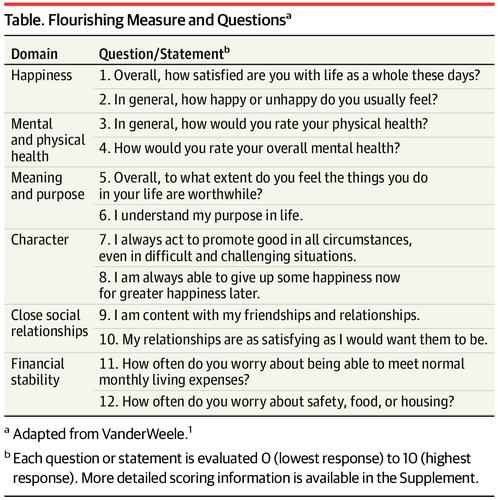
“How should we define ‘health?'” a 2011 BMJ article asked. The context for the question was that the 1948 World Health Organization definition of health — that health is, “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”– was not so useful in the 21st century. The authors, a global, multidisciplinary team from Europe, Canada and the U.S., asserted that by 2011, human health was marked less by infectious disease and more by non-communicable conditions that could be highly influenced, reversed and prevented through self-care by the individual and public health policy
How Consumers’ Belt-Tightening Could Impact Health/Care – Insights from Deloitte’s Retail Team

Over the ten years between 2007 and 2017, U.S. consumer spending for education, food and health care substantially grew, crowding out spending for other categories like transportation and housing. Furthermore, income disparity between wealthy Americans and people earning lower-incomes dramatically widened: between 2007-2017, income for high-income earners grew 1,305 percent more than lower-incomes. These two statistics set the kitchen table for spending in and beyond 2019, particularly for younger people living in America, considered in Deloitte’s report, The consumer is changing, but perhaps not how you think. The authors are part of Deloitte Consulting’s Retail team. The retail spending data
How Consumers Look At Social Determinants of Health for Cancer, Diabetes and Mental Health

Enlightened health/care industry and public policy stakeholders have begun to embrace and address social determinants of health. These are the inputs that bolster health beyond health care services: they include economic stability like job security and income level (and equity), education, and access to healthy food, food security, safe neighborhoods, social support, clean environments (water and air), and in my own update on SDoH factors, access to broadband connectivity. As physician leaders in the AMA, technology advocates from AMIA, and numerous health plans focus efforts on strengthening social determinants, what do people – consumers, patients, caregivers — think about these
Patients’ Expectations for Health Beyond Care: Think Food, Exercise, Emotions, Sleep and Finance

People want to make health with their health care providers, and they want more than care from them: most patients are looking for support with healthy eating, exercise, emotional support, sleep, stress management, social relationships, and financial health. And in case physicians, nurses and pharmacists aren’t sufficiently business with that punch-list for health, two in three U.S. patients would also like to receive help in finding a higher purpose. This is the health consumer’s mass call-out for holistic health, Welltok discovered in a survey conducted among over 1,600 U.S. adults in March 2019. The results are detailed in the assertively
Two-Thirds of Americans Say Healthcare Doesn’t Work Well, in RealClear Politics Poll

Health care is the top issue facing the U.S. today, one in three Americans says, with another one-fourth pointing to the economy. Together, health care + the economy rank the top issues for 62% of Americans. Health care and the economy are, in fact, intimately tied in every American’s personal household economy I assert in my book, HealthConsuming: From Health Consumer to Health Citizen. This poll from RealClear Politics, conducted in late April/early May 2019, makes my point that the patient is the consumer and, facing deductibles and more financial exposure to footing the medical bill, the payor. Fully
The 3 A’s That Millennials Want From Healthcare: Affordability, Accessibility, Availability

With lower expectations of and satisfaction with health care, Millennials in America seek three things: available, accessible, and affordable services, research from the Transamerica Center for Health Studies has found. Far and away the top reason for not obtaining health insurance in 2018 was that it was simply too expensive, cited by 60% of Millennials. Following that, 26% of Millennials noted that paying the tax penalty plus personal medical expenses were, together, less expensive than available health options. While Millennials were least likely to visit a doctor’s office in the past year, they had the most likelihood of making a
Scaling the Social Determinants of Health – McKinsey and Kaiser’s Bold Move

People who are in poor health or use more health care services are more likely to report multiple unmet social needs, such as food insecurity, unsafe neighborhoods, lack of good housing, social isolation, and poor transportation access, found through a survey conducted by McKinsey. The results are summarized in Addressing the Social Determinants of Health. The growing recognition of the influence of social determinants reached a tipping point last week with the news that Kaiser-Permanente would work with Unite US to scale services to people who need them. The mainstreaming of SDoH speaks to the awareness that health is made
Assessing the GAO’s Report on Single-Payer Healthcare in America: Let’s Re-Imagine Workflow

Calls for universal health care, some under the banner of Medicare for All,” are growing among some policy makers and presidential candidates looking to run in 2020. As a response, the Chairman of the House Budget Committee in the U.S. Congress, Rep. John Yarmuth (D-Ky.), asked the Congressional Budget Office (CBO) to develop a report outlining definitions and concepts for a single-payer health care system in the U.S. The result of this ask is the report, Key Design Components and Considerations for Establishing a Single-Payer Health Care System, published on 1st May by the CBO. The report provides
Will Health Consumers Morph Into Health Citizens? HealthConsuming Explains, Part 5

The last chapter (8) of HealthConsuming considers whether Americans can become “health citizens.” “Citizens” in this sense goes back to the Ancient Greeks: I return to Hippocrates, whose name is, of course, the root of The Hippocratic Oath that physicians take. Greece was the birthplace of Democracy with a capital “D.” Hippocrates’ book The Corpus is thought to be one of the first medical textbooks. The text covered social, physical, and nutritional influences, and the concept of “place” for health and well-being. Here, the discussion detailed the roles of air and water for health. The Hippocratic texts also coached doctors to
What We Know We Know About ZIP Codes, Food, and Deaths of Despair – HealthConsuming Explains, Part 3

“There’s a 15-year difference in the life expectancy between the richest and poorest Americans.” That’s the first sentence of Chapter 7 in my book, HealthConsuming: From Health Consumer to Health Citizen. This data point comes from research published in JAMA in April 2016 on the association between income and life expectancy in the U.S. (That’s endnote #399 in the back of the book, one of 519 notes I use to support the plotline). Today, the Brookings Institution convened a meeting on the funding for social determinants of health to address disparities, costs, and quality of healthcare in America. The overall
Health Consumers Are Now Amazon-Primed for Healthcare – HealthConsuming Explains, Part 2
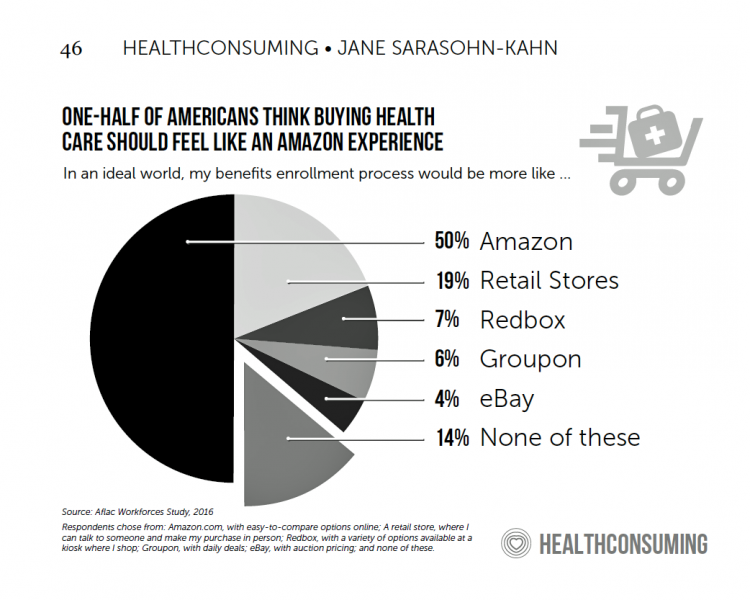
As patients now assume the role of health consumer, they rationally expect retail-level experiences with greater first-dollar payment for health insurance, health care services and medical products like prescription drugs. Consumers know what good retail looks and feels like, and are focusing that experiential lens on health care, Aflac found when their Workforces Survey polled Americans on their desirable health insurance shopping experience. One in two people said it should feel, “like Amazon,” and another 20% of folks said, “like retail.” Chapter 3 of HealthConsuming is titled, “How Amazon Has Primed Health Consumers,” and explains this re-shaping of patient expectations.
A Dose of Optimism Is a Prescription for Financial Health, Says Frost Bank

People define their personal health and well-being broadly, well beyond physical health. Mental wellness, physical appearance, social connections, and financial wellness all add into our self-health definitions. Mind Over Money is a consumer study conducted by Frost Bank, working with FleischmanHillard, connecting the dots between optimism and financial health. The top-line of the study is that people who are optimists have roughly two-thirds fewer days of financial stress per year than pessimists. Put another way, pessimists stress about finances 62% of the year, shown in the first chart from the study. This translates into 62% of optimists having better financial
Americans’ Trust in U.S. Healthcare Lags Tech — and Women Are Particularly Cynical
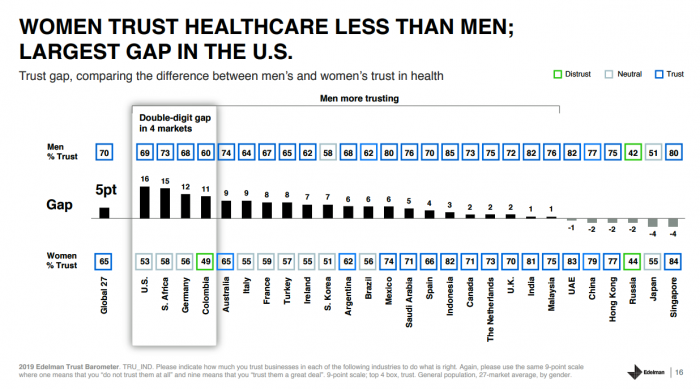
The 2019 Edelman Trust Barometer measured the biggest gap in trust for the healthcare industry between the U.S. “informed public” and the mass population. Fewer American women, too, trust the healthcare industry than men do. “This inequality of trust may be reflective of the mass population continuing to feel left behind as compared to others, even as they recognize the advances that are being made that could benefit them. Given tone and tenor of the day, and particularly among mass population, healthcare may continue to see increasing demands for change and regulation,” Susan Isenberg, Edelman’s head of healthcare, notes in
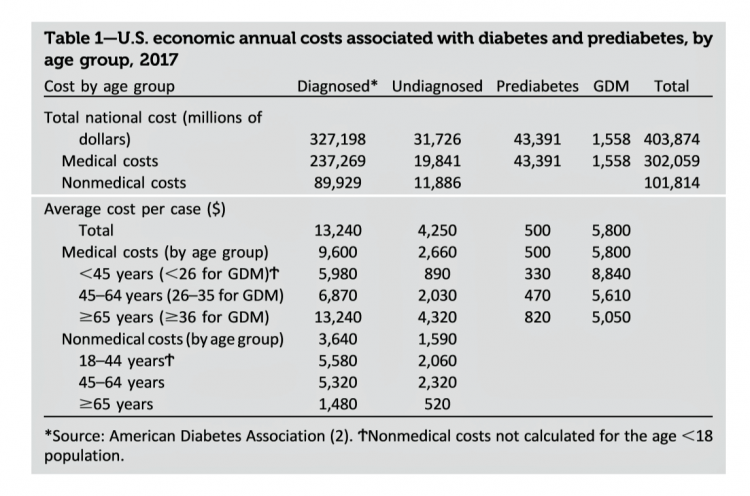
The United States of Diabetes: a $1,240 Tax on Every American
Pharmaceutical company executives are testifying in the U.S. Congress this week on the topic of prescription drug costs. One of those medicines, insulin, cost a patient $5,705 for a year’s supply in 2016, double what it cost in 2012, according to the Health Care Cost Institute. Know that one of these insulin products, Lilly’s Humalog, came onto the market in 1996. In typical markets, as products mature and get mass adoption, prices fall. Not so insulin, one of the many cost components in caring for diabetes. But then prescription drug pricing doesn’t conform with how typical markets work in theory.
World Health Day 2019: Let’s Celebrate Food, Climate, Insurance Coverage and Connectivity
Today, 7 April, is World Health Day. With that in mind, I devote this post to three key social determinants of health (SDOH) that are top-of-mind for me these days: food for health, climate change, and universal health coverage. UHC happens to be WHO’s focus for World Health Day 2019. [As a bonus, I’ll add in a fourth SDOH in the Hot Points for good measure and health-making]. Why a World Health Day? you may be asking. WHO says it’s, “a chance to celebrate health and remind world leaders that everyone should be able to access the health care they need,
Medical Costs Are Consuming Americans’ Financial Health
Spending on medical care costs crowded out other household spending for millions of Americans in 2018, based on The U.S. Healthcare Cost Crisis, a survey from West Health and Gallup. Gallup polled 3,537 U.S. adults 18 and over in January and February 2019. One in three Americans overall are concerned they won’t be able to pay for health care services or prescription drugs: that includes 35% of people who are insured, and 63% of those who do not have insurance. Americans borrowed $88 billion in 2018 to pay for health care spending, West Health and Gallup estimated. 27 million Americans
In the U.S., Patients Consider Costs and Insurance Essential to Their Overall Health Experience
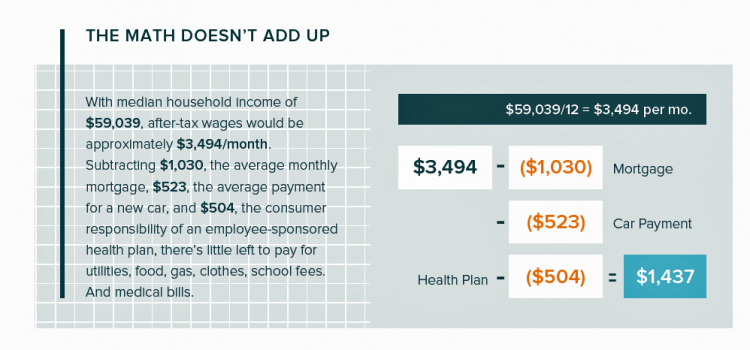
Patients in the U.S. assume the role of payor when they are enrolled in high-deductible health plans. People are also the payor when dealing with paying greater co-payments for prescription drugs, especially as new therapeutic innovations come out of pipelines into commercial markets bearing six-digit prices for oncology and other categories. For mainstream Americans, “the math doesn’t add up” for paying medical bills out of median household budgets, based on the calculations in the 2019 VisitPay Report. Given a $60K median U.S. income and average monthly mortgage and auto payments, there’s not much consumer margin to cover food, utilities, petrol,
Medical Issues Are Still The #1 Contributor to Bankruptcy in the U.S., An AJPH Study Asserts
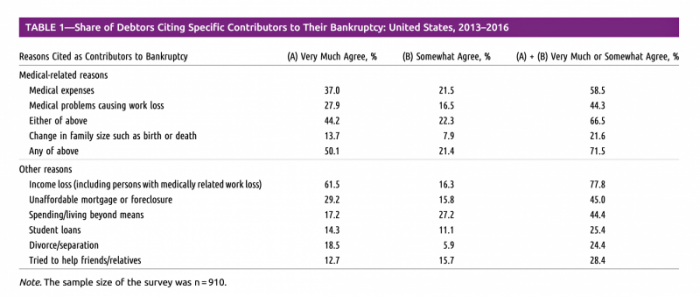
Medical costs in America are still the top contributor to personal bankruptcy in the U.S., a risk factor in two-thirds of bankruptcies filed between 2013 and 2016. That’s a sad fiscal fact, especially as more Americans gained access to health insurance under the Affordable Care Act, according to a study published this month in the American Journal of Public Health (AJPA). Between 2013 and 2016, about 530,000 bankruptcies were filed among U.S. families each year associated with medical reasons, illustrated in Table 1 from the study. The report, Medical Bankruptcy: Still Common Despite the Affordable Care Act, updates research from 2007 which
Most Americans Across Party ID Favor U.S. Government Negotiation to Lower Rx Drug Costs

There’s little Americans, by political party, agree upon in 2019. One of the only issues bringing people together in the U.S. is prescription drug prices — that they’re too high, that the Federal government should negotiate to lower costs for Medicare enrollees, and that out-of-pocket costs for drugs should be limited. The Kaiser Family Foundation has been tracking this topic for a few years, and this month, their March 2019 Health Tracking Poll shows vast majorities of Democrats, Independents and Republicans all share these sentiments. It’s not that patients who take prescription drugs don’t appreciate them – most (58%) say medicines
National Health Spending Will Reach Nearly 20% of U.S. GDP By 2027
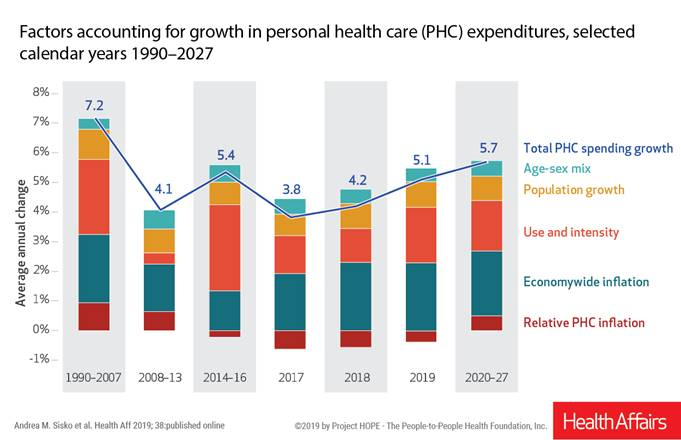
National health spending in the U.S. is expected to grow by 5.7% every year from 2020 to 2027, the actuaries at the Centers for Medicare and Medicaid Services forecast in their report, National Health Expenditure Projections, 2018-2927: Economic And Demographic Trends Drive Spending And Enrollment Growth, published yesterday by Health Affairs. For context, note that general price inflation in the U.S. was 1.6% for the 12 months ending January 2019 according to the U.S. Bureau of Labor Statistics. This growth rate for health care costs exceeds every period measured since the high of 7.2% recorded in 1990-2007. The bar chart illustrates the
Open Table for Health: Patients Are Online For Health Search and Physician Reviews
Seeking health information online along with researching other patients’ perspectives on doctors are now as common as booking dinner reservations and reading restaurant reviews, based on Rock Health’s latest health consumer survey, Beyond Wellness for the Healthy: Digital Health Consumer Adoption 2018. Rock Health has gauged consumes’ digital health adoption fo a few years, showing year-on-year growth for “Googling” health information, seeking peer patients’ physician and hospital reviews, tracking activity, donning wearable tech, and engaging in live telehealth consultations with providers, as the first chart shows. The growth of tracking and wearable tech is moving toward more medical applications beyond fitness
Health Is Social – The Social Determinants of Health at HIMSS19
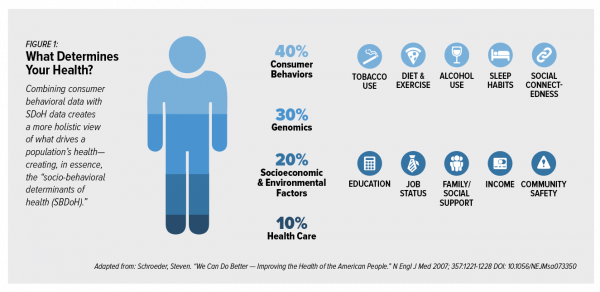
In the health care world, it is now commonly accepted that genes contribute less than half of the influence on peoples’ health status. Other issues play starring roles in overall well-being, including environmental factors, health care services, and social determinants of health (SDOH). These inputs include education, personal economics (like job security and financial stability), physical built environments (think: transportation access, safe and healthy housing), food and nutrition, and access to health care. At HIMSS17, I gave a talk in a big room about how technology can scale SDOH; we had standing room only, which is not a brag —
The Cost of Prescription Drugs, Doctors and Patient Access – A View from HIMSS19
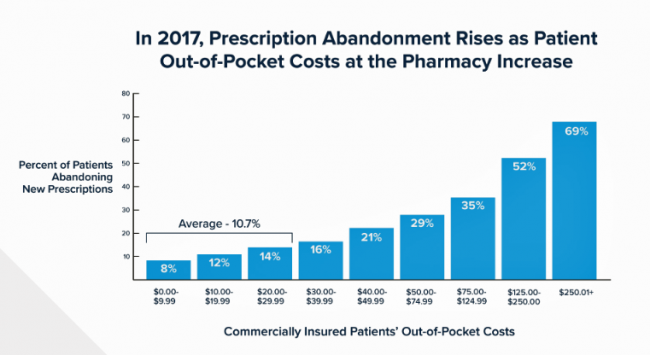
Most patient visits to doctors result in a prescription written for a medicine that people retrieve from a pharmacy, whether retail in the local community or via mail order for a maintenance drug. This one transaction generates a lot of data points, which individually have a lot of importance for the individual patient. Mashed with other patients’, prescription drug utilization data can combine with more data to be used for population health, cost-effectiveness, and other constructive research pursuits. At HIMSS19, there’s an entire day devoted to a Pharma Forum on Tuesday 12 February, focusing on pharma-provider-payor collaborations. Allocating a full
The Expectation Gap Between What Patients Want Vs What They Get
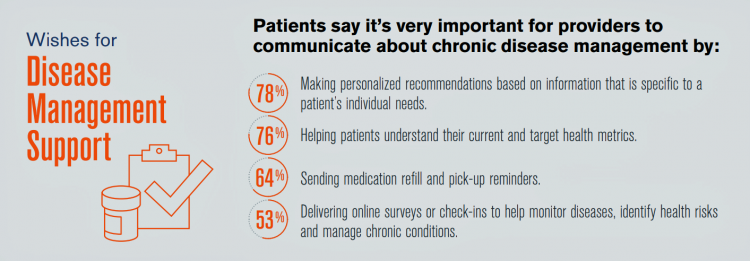
Talk to me, patients are demanding in unison. Most health consumers expect providers to communicate about routine health care and prevention; this is especially true among those patients trying to manage chronic conditions we learn from 10 Ways to Fulfill Patients’ Communication Wish List, a report based on a consumer survey from West, the communications and network infrastructure company. Four in five patients say that talking to “me” means they want personalized recommendations to their unique needs – but only one-third of patients say they’re getting that level of service from their healthcare providers. Most health consumers expect providers to communicate about
Care Gets Personal at Philips for Parents and Babies

Our homes should nurture our health. In addition to nutrition and good food, positive relationships, clean air and water, and the basic needs that bolster whole health, technology is playing a growing role to help us manage health at home. At CES 2019, I spent time with Roy Jakobs, Chief Business Leader of Personal Health with Philips, to discuss the company’s evolving portfolio of products that help fulfill the mission to support people across their own continuum of health. Following CES, I wanted to further dive into one part of the portfolio very important to family health at home: the
Calling Out Health Equity on Martin Luther King Day 2019
On this weekend as we appreciate the legacy of Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would deliver two months later in Washington, DC. Wisdom from the speech: “But now more than ever before, America is forced to grapple with this problem, for the shape of the world today does not afford us the luxury of an anemic democracy. The price that this nation must pay for the continued oppression and exploitation of the Negro or any other
In U.S. Health Care, It’s Still the Prices, Stupid – But Transparency and Consumer Behavior Aren’t Working As Planned
I’m glad to be getting back to health economic issues after spending the last couple of weeks firmly focused on consumers, digital health technologies and CES 2019. There’s a lot for me to address concerning health care costs based on news and research published over the past couple of weeks. We’ll start with the centerpiece that will provide the overall context for this post: that’s the ongoing research of Gerard Anderson and colleagues under the title, It’s Still The Prices, Stupid: Why The US Spends So Much On Health Care, And A Tribute To Uwe Reinhardt. It is bittersweet to
The Caveats for Health/Care at CES 2019

According to the Cambridge Dictionary, a “caveat” is, “a warning to consider something before doing anything more.” It is fitting that CES is held in Las Vegas, land of high risk and, with a lot of luck, reward. With that theme in mind, I depart LAS airport tonight on an aptly-named red-eye flight back home after spending an entire week here. I’m pondering not what I saw — some of which I covered daily over the past week — but what I didn’t see. Consider these the caveats for health/care at #CES2019. In no particular order… Where was the Chairman of
The Consumer as Payor – Retail Health at CES 2019

All health/care is retail now in America. I say this as most people in the U.S. who have health insurance must take on a deductible of some amount, which compels that insured individual to spend the first dollar on medical services up until they meet their financial commitment. At that point, health insurance kicks in, and then the insured may have to spend additional funds on co-payments for general medicines and services, and coinsurance for specialty drugs like injectables and high-cost new therapies. The patient is a consumer is a payor, I asserted today during my talk on the expanding
Costs, Consumerism, Cyber and Care, Everywhere – The 2019 Health Populi TrendCast

Today is Boxing Day and St. Stephens Day for people who celebrate Christmas, so I share this post as a holiday gift with well-wishes for you and those you love. The tea leaves have been brewing here at THINK-Health as we prepared our 2019 forecast at the convergence of consumers, health, and technology. Here’s our trend-weaving of 4 C’s for 2019: costs, consumerism, cyber and care, everywhere… Health care costs will continue to be a mainstream pocketbook issue for patients and caregivers, with consequences for payors, suppliers and ultimately, policymakers. Legislators inside the DC Beltway will be challenged by the
While National Health Care Spending Growth Slowed in 2017, One Stakeholder’s Financial Burden Grew: The Consumer’s

National health care spending growth slowed in 2017 to the post-recession rate of 3.9%, down from 4.8% in 2016. Per person, spending on health care grew 3.2% to $10,739 in 2017, and the share of GDP spent on medical care held steady at 17.9%. Healthcare spending in America is a $3.5 trillion micro-economy…roughly the size of the entire GDP of Germany, and about $1 trillion greater than the entire economy of France. These annual numbers come out of the annual report from the Centers for Medicare and Medicaid Services, published yesterday in Health Affairs. Underneath these macro-health economic numbers is
Most Americans Want the Federal Government to Ensure Healthcare for All

Most people in the U.S. believe that the Federal government should ensure that their fellow Americans, a new Gallup Poll found. This sentiment has been relatively stable since 2000 except for two big outlying years: a spike of 69% in 2006, and a low-point in 2003 of 42%. In 2006, Medicare Part D launched, which may have boosted consumers’ faith in Federal healthcare programs. In contrast, in 2013 the Affordable Care Act was in implementation and consumer-adoption mode, accompanied by aggressive anti-“Obamacare” campaigns in mass media. That’s the top lighter green line in the first chart. But while there’s majority support
Money First, Then Kids: The State of the American Family in 2018

Most American families with children at home are concerned about paying bills on a monthly basis. One in two people have had at least one personal “economic crisis” in the past year, we learn in the American Family Survey 2018, released last week from Deseret News and The Brookings Institution. The project surveyed 3,000 U.S. adults across the general population, fielded online by YouGov. This poll, conducted since 2005, looks at the state of U.S. families through several issue lenses: the state of marriage and family, parents and teenagers, sexual harassment (with 2018 birthing the #MeToo movement), social capital and
The Ultimate Health Outcome, Mortality, Is Rising in America

How long can people living in the U.S. expect to live? 78.6 years of age, if you were born in 2017. That’s a decline of 0.1 year from 2016. This decline especially impacted baby boys: their life expectancy fell to 76.1 years, while baby girls’ life expectancy stayed even at 81.1 years. That’s the latest data on Mortality in the United States, 2017, soberly brought to you by the Centers for Disease Control and Prevention, part of the U.S. Department of Health and Human Services. Underneath these stark numbers are the specific causes of death: in 2017, more Americans died
Data Privacy and Healthcare Access: Top Issues Shaping Consumers’ Societal ROI

Organizations that address consumers’ data privacy and access to healthcare create greater social brand equity, inspiring people to say nice things about the companies, recommend them as good employers, and be welcomed as businesses operating in peoples’ community. In The Societal ROI Index: A Measure for The Times We Find Ourselves In, Finn Partners and The Harris Poll measure U.S. companies’ reputations for social good, the project’s press release explains. “Our new data shows that the public has a definite opinion about what issues they feel companies should address and the social impact bar has been set high,” according to Amy Terpeluk,





 Thank you, Jared Johnson, for including me on the list of the
Thank you, Jared Johnson, for including me on the list of the  I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,
I am so grateful to Tom Lawry for asking me to pen the foreword for his book, Health Care Nation,  Thanks to Feedspot for naming this blog, Health Populi, as a
Thanks to Feedspot for naming this blog, Health Populi, as a