National Health Spending in the U.S. in 2033: What 20.3% of the GDP Will Be Spent On
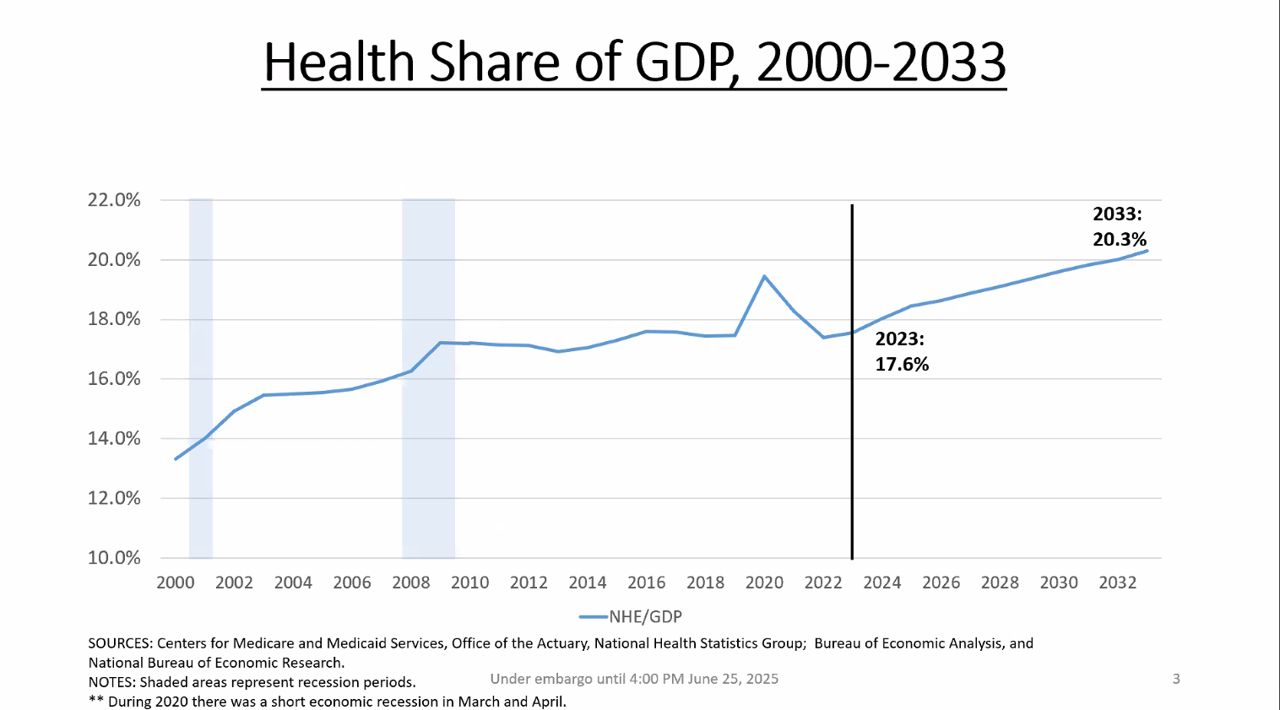
By 2033, national health spending will comprise 20.3% of the U.S. GDP, based on the latest national health expenditure projections developed by researchers from the Centers for Medicare and Medicaid Services (CMS). This growth will be happening as CMS projects coverage of insured people to decline over the period. Earlier today, I attended a media briefing hosted by Health Affairs to receive the CMS team’s top-line forecast of NHE from 2024 to 2033 discussing these findings. Fuller details on the projections will be released in the July issue of Health Affairs on 7
Americans’ Trust in Public Health Agencies Has Become Politicized, Though There is Bipartisan Support for Many Public Health Priorities

While health citizens’ trust in the “messengers” of health information has become polarized by partisans’ political views, there is real concordance of support for many public health priorities. We weave together two current studies to come to this realization: the latest (April 2025) KFF Tracking Poll on Health Information and Trust, KFF’s ongoing health survey (published 6 May); and, the de Beaumont – Harvard Chan School of Public Health poll into Americans’ views on public health in “the first 100 days” of President Trump’s presidency. First, consider the KFF study, conducted among
The Biggest Opportunity for Sporting Goods is Consumers’ Physical Inactivity: Learning from McKinsey (with a personal nod to pickleball)

McKinsey just published a detailed report into Sporting Goods 2025, which the firm calls a “new balancing act” that must turn uncertainty into opportunity. The report is based on five key observations: Only a few sporting goods companies have expanded growth and margins since 2018 — and must “rethink the value chain” in the face of challenging geopolitical headwinds One-half of so-called “active consumers” say that fitness is a core element of their identity, with emotional connections to brands they purchase for the lifestyle Incumbent sporting goods companies are losing market share to
What is a Consumer Health Company? Riffing Off of Deloitte’s Report on CHCs/A 2Q2025 Look at Self-Care Futures
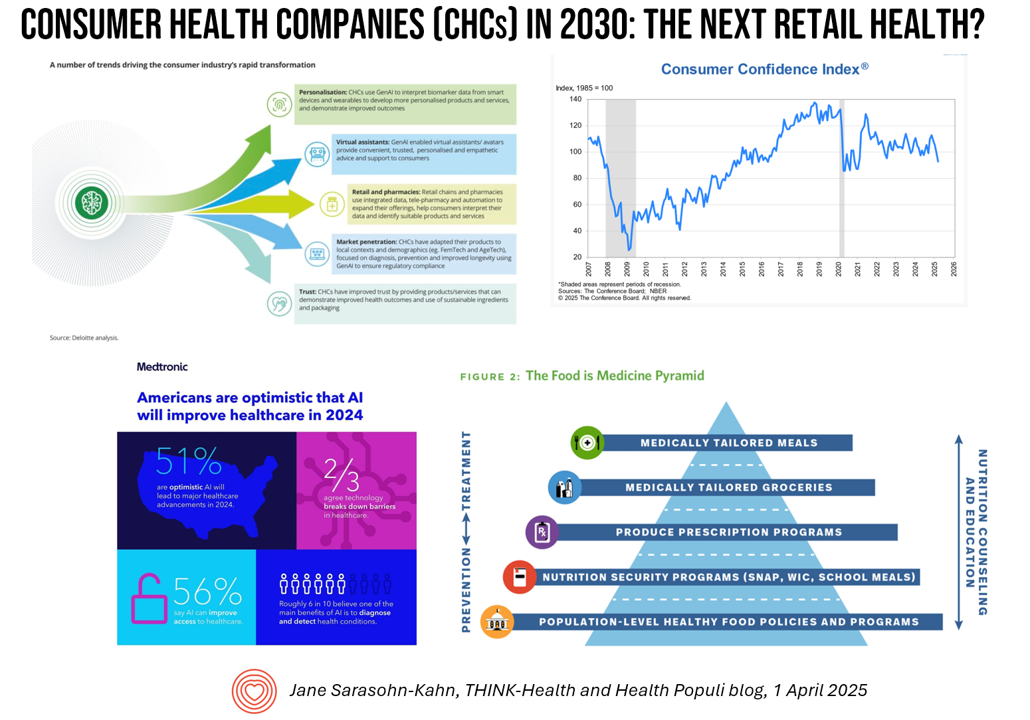
The health care landscape in 2030 will feature an expanded consumer health industry that will become, “an established branch of the health ecosystem focused on promoting health, preventing, disease, treating symptoms and extending healthy longevity,” according to a report published by Deloitte in September 2024, Accelerating the future: The rise of a dynamic consumer health market. While this report hit the virtual bookshelf about six months ago, I am revisiting it on this first day of the second quarter of 2025 because of its salience in this moment of uncertainties across our professional and personal lives — particularly related to
One Way to Improve U.S. Healthcare, Lower Costs and Drive Outcomes? “Unvendor,” Asserts Dr. Harm Scherpbier in His New Book

Health information technology professionals charged with selecting, implementing, updating, and paying for health IT in hospital and care delivery settings are essentially the first-line “consumers” of health IT – specifically, electronic health records. But these health IT leaders feel far from empowered and choiceful as consumers in todays EHR vendor “monoculture,” Harm Scherpbier, MD, explains in his book, Unvendor. I spent time with Harm to discuss the book, its backstory, and what he hopes to accomplish by raising the issue of single-vendor health IT and how clinicians, health IT staff, and
Think Quintuple Aim This Week at #HIMSS25
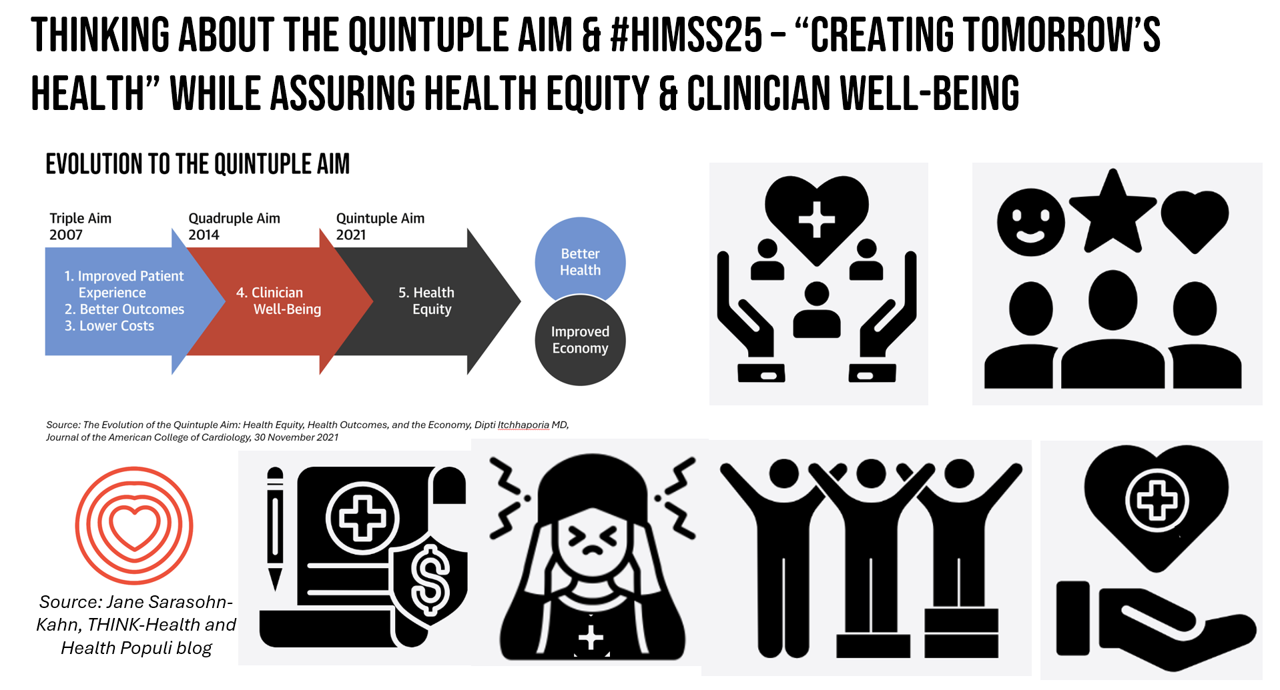
As HIMSS 2025, the largest annual conference on health information and innovation meets up in Las Vegas this week, we can peek into what’s on the organization’s CEO’s mind leading up to the meeting in this conversation between Hal Wolf, CEO of HIMSS, and Gil Bashe, Managing Director of FINN Partners. If you are unfamiliar with HIMSS, Hal explains in the discussion that HIMSS’s four focuses are digital health transformation, the deployment and utilization of AI as a tool, cybersecurity to protect peoples’ personal information and its use, and, workforce development. I have my own research agenda(s) underneath these themes
COVID-19 Further Splits American Society as Trust Continues to Erode – a 5-Year Perspective from Pew
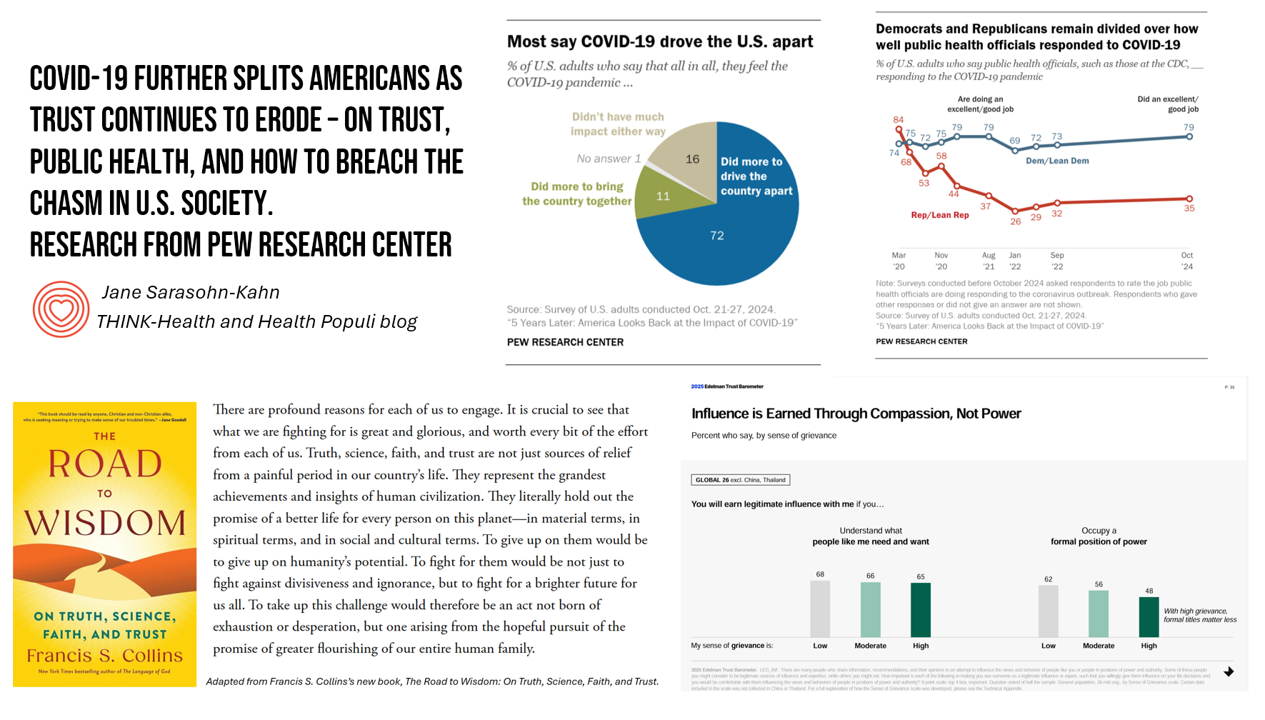
The partisan divide in the U.S., exacerbated by the COVID-19 pandemic, could set the stage for another public health emergency given eroding trust in institutions — especially in media, government, and public health officials. I base this sobering forecast on the latest study from the Pew Research Center which polled people in the U.S. about their pandemic-perspectives, detailed in the report 5 Years Later: America Looks Back at the Impact of COVID-19. Couple these findings with the recent dismissal of public health “disease detectors” working with the Centers for Disease Control (CDC), and what is currently termed a “quademic” (that
Health/Care at Super Bowl LIX, GLP-1s, Kaiser and Tufts on Food-As-Medicine, and the RFK, Jr. Factor: A Health Consumer Check-In

In the wake of the always-creative ads for Super Bowl and last Sunday’s LIX bout, game-watchers got to see a plethora of commercials dedicated to the annual event’s major features: food and game-day eating. Oh, and what’s turned out to be the most controversial commercial, the one on GLP-1s from Hims & Hers. In that vein, and converging with many news and policy events, I’m trend-weaving the latest insights into that most consumer-facing of the social determinants of health: food, and in particular, health consumers viewing and adopting food as part of their health and well-being moves. First, to the
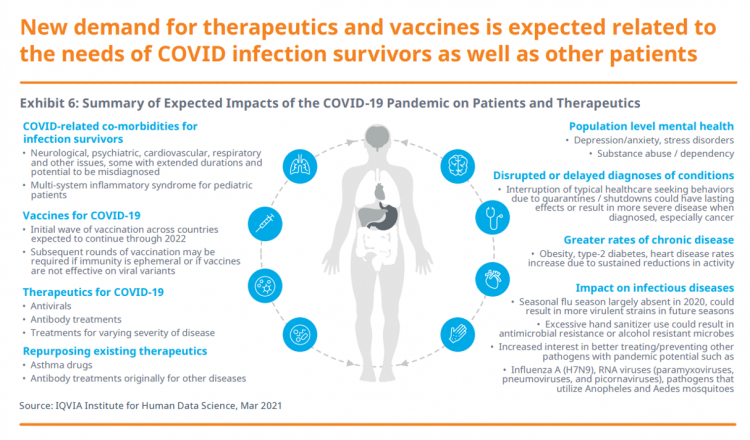
Measuring Progress for Life Sciences: Trust, Patient Access, and Prevention at a Fork in the Road of Public Health
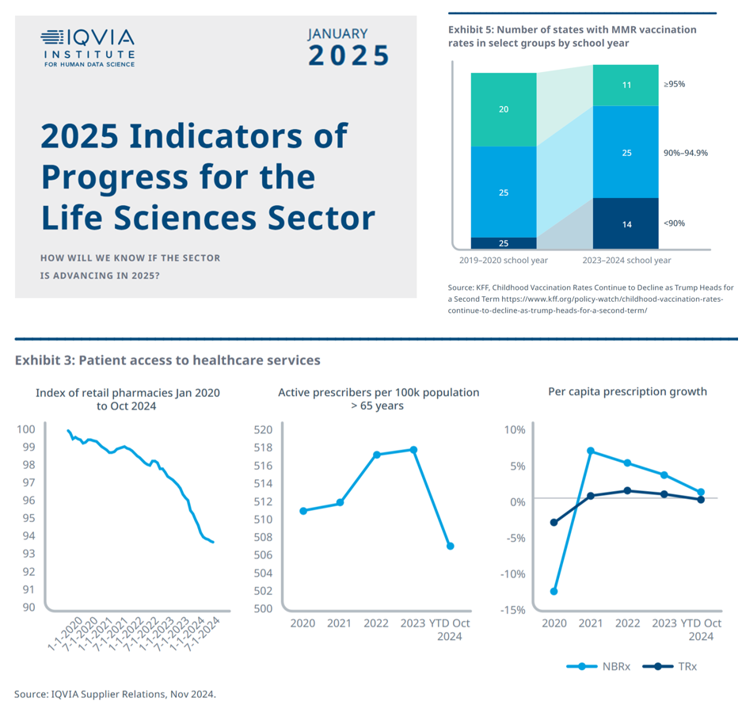
How will we know if the life sciences sector is advancing in 2025? This is the question asked at the start of the report, a Research Brief: 2025 Indicators of Progress for the Life Sciences Sector, from the IQVIA Institute for Human Data Science (IQVIA). To answer that question, IQVIA identified ten indicators for this 2025 profile on the life sciences sector. I selected four key data points for this discussion which provide particularly informative insights for my advisory work right now at the intersection of health, people/consumers, and technology: Trust for/with/in life science
There’s a Health Gap for Women Around the World – and the World Economic Forum Has a Blueprint to Fix It
Even though women comprise one-half of the world’s population, their health outcomes and inputs do not match up to men’s: there’s a women’s health gap on Planet Earth. Meeting in Davos this week for #WEF2025, the World Economic Forum published a report on that gender-health chasm titled, Blueprint to Close the Women’s Health Gap: How to Improve Lives and Economies for All. In collaboration with the McKinsey Health Institute, the report focuses on nine key conditions that, if addressed, could reduce the global disease burden by 27 million disability adjusted life years and add
Most People in the U.S. Trust the CDC and NIH for Health Information, and Most Want President Trump to Strengthen Health Institutions
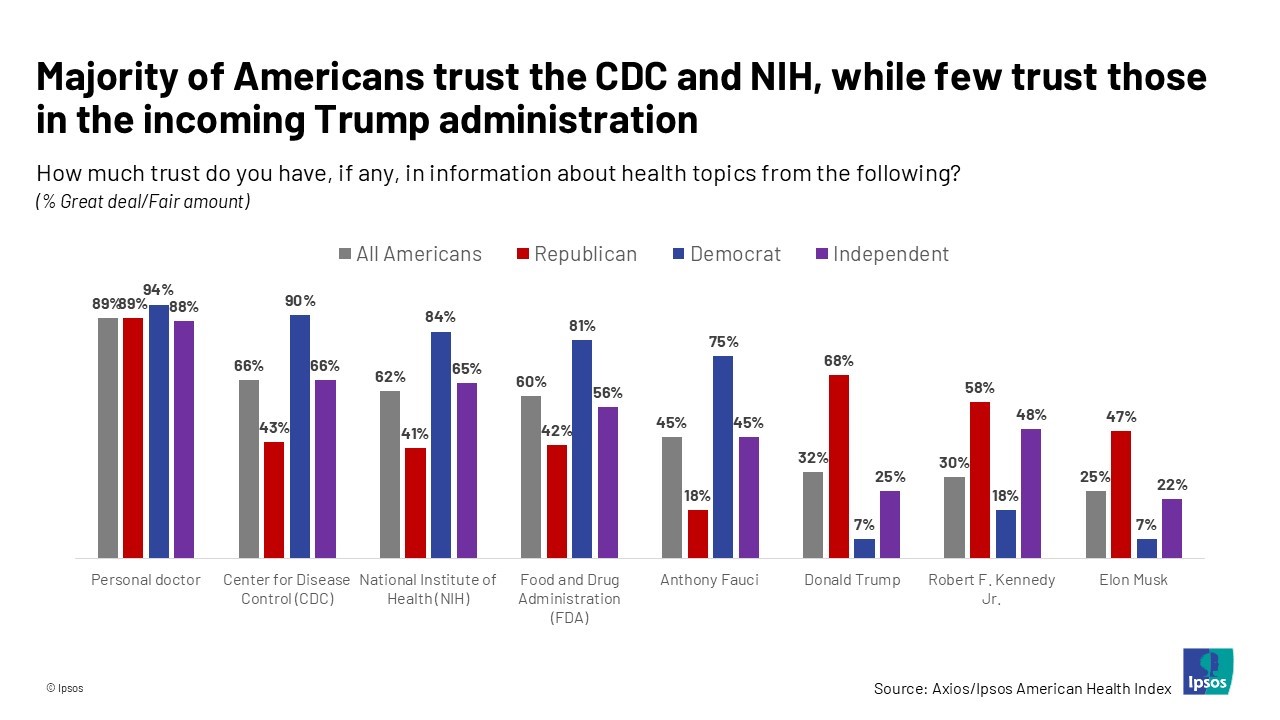
Most health citizens in the U.S. trust the CDC, NIH, and FDA, and most people also want the 47th incoming President Donald Trump to strengthen health/care institutions — from the VA and FDA to Medicare, Medicaid, as well as the CDC and Affordable Care Act. The Axios/Ipsos American Health Index, published this week, reveals both concurrence among U.S. health consumers with some striking differences across political party ID. Axios and Ipsos fielded a survey among 1,002 U.S. adults in early December to glean peoples’ perspectives on health, trust, and a variety of health and social policies.
Workers Feel “Stuck,” Under-Insured, Financially Stressed, and Neglecting Mental Health
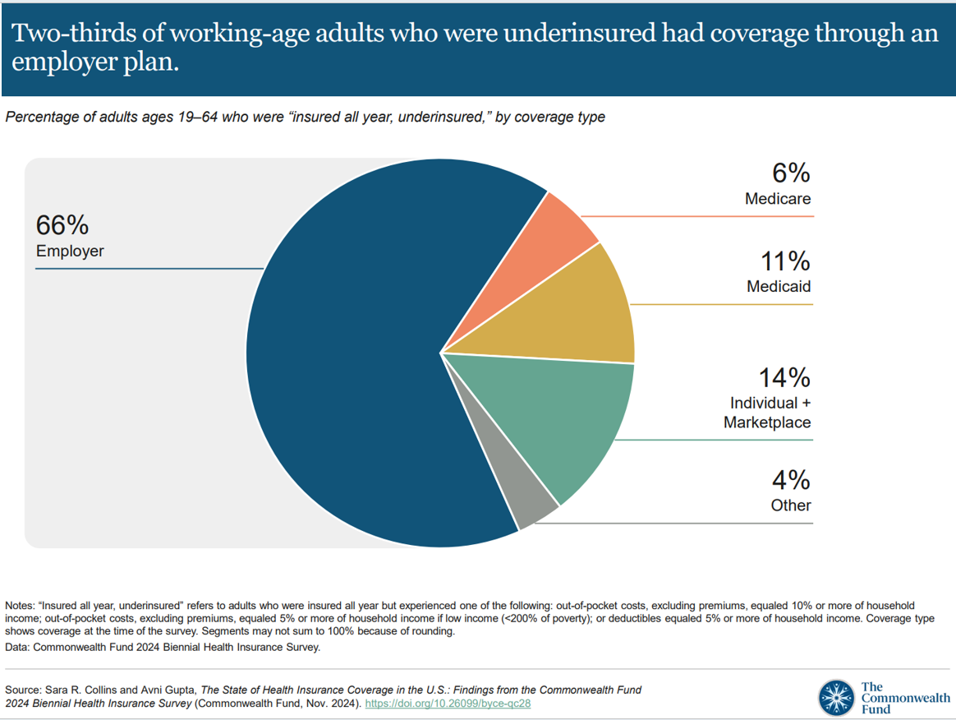
“It’s the economy stupid,” Jennifer Tescher, CEO of the Financial Health Network, titles her latest column in Forbes. Published two weeks after the 2024 U.S. elections, Jennifer’s assertion sums up what, ex post facto, we know about what most inspired American voters at the polls in November 2024: the economy, economics, inflation, the costs of daily living….pick your noun, but it’s all about those Benjamins right now for mainstream American consumers across many demographic cuts. With that realization, we must remind ourselves as we enter a new year under a second-term President Trump that health care spending for everyday people
1 in 2 U.S. Women (“The Bedrock of Society”) Self-Ration Care – the Latest Deloitte Findings
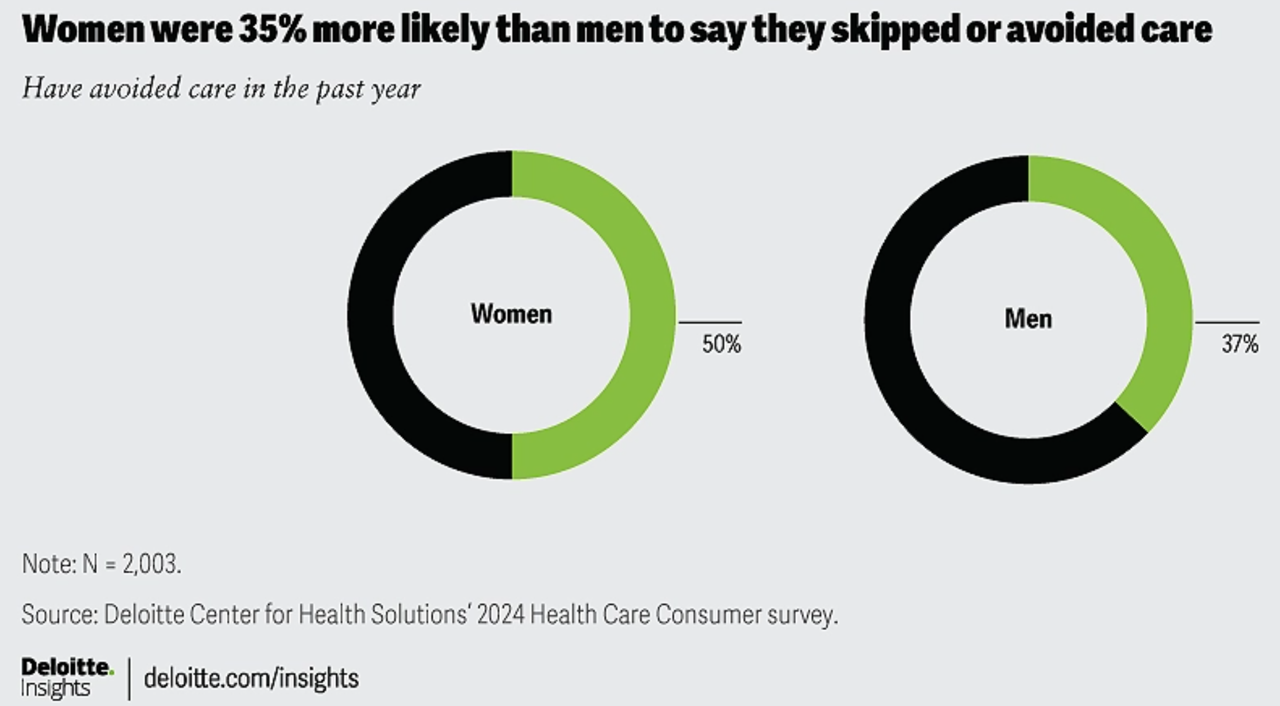
Women in the U.S. are more likely to avoid care than men in America, Deloitte found in the consulting firm’s latest survey on consumers and health care. Deloitte coins this phenomenon as a “triple-threat” that women face in the U.S. health care environment, the 3 “threats” being, Affordability, Access, and, Prior experience — that is the health disparity among women who have seen personal mis-diagnosis, bias, or treatment that hasn’t been consistent with current protocols and practices. The data come out of Deloitte’s fielding of the U.S. consumer survey in February and March, 2024.
How Voting Plays Into Health, Health Equity, and Community Well-Being

“Voter registration in hospitals is the new frontier in health care.” That’s the headline in a WBUR story last week detailing the efforts of health care professionals in “amplifying” their patients’ voices inside and outside of the hospital walls by advocating for their health citizenship — through voter registration and public health policy advocacy. I’m a long-time evangelist for health citizenship and the role that a person’s engagement in the civic commons plays in one’s own health, the health of their communities and of the nation as a whole. I’m not alone
Women’s Health Outcomes in the U.S.: Spending More, Getting (Way) Less – 4 Charts from The Commonwealth Fund
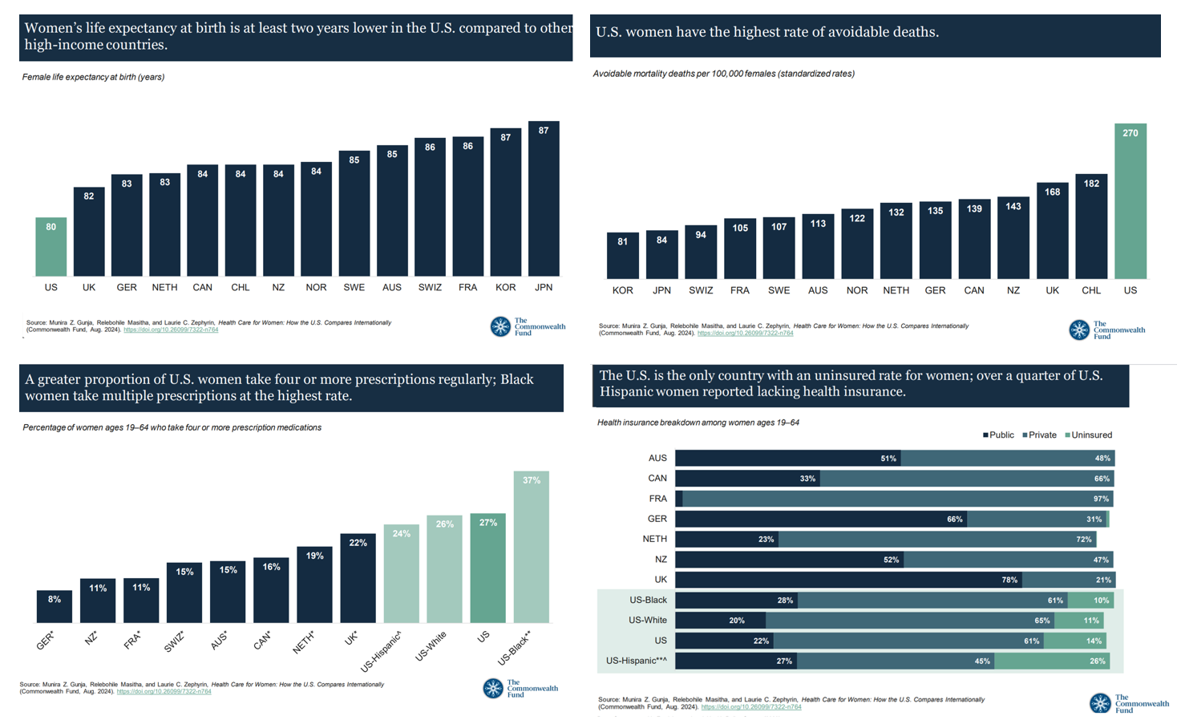
Women in the U.S. have lower life expectancy, greater risks of heart disease, and more likely to face medical bills and self-rationing due to costs, we learn in the latest look into Health Care for Women: How the U.S. Compares Internationally from The Commonwealth Fund. The Fund identified four key conclusions in this global study: Mortality, shown in the first chart which illustrates women in the U.S. having the lowest life expectancy of 80 years versus women in other high-income countries; Health status, with women in the U.S. more likely to consume multiple prescription
Healthcare 2030: Are We Consumers, CEOs, Health Citizens, or Castaways? 4 Scenarios On the Future of Health Care and Who We Are – Part 1
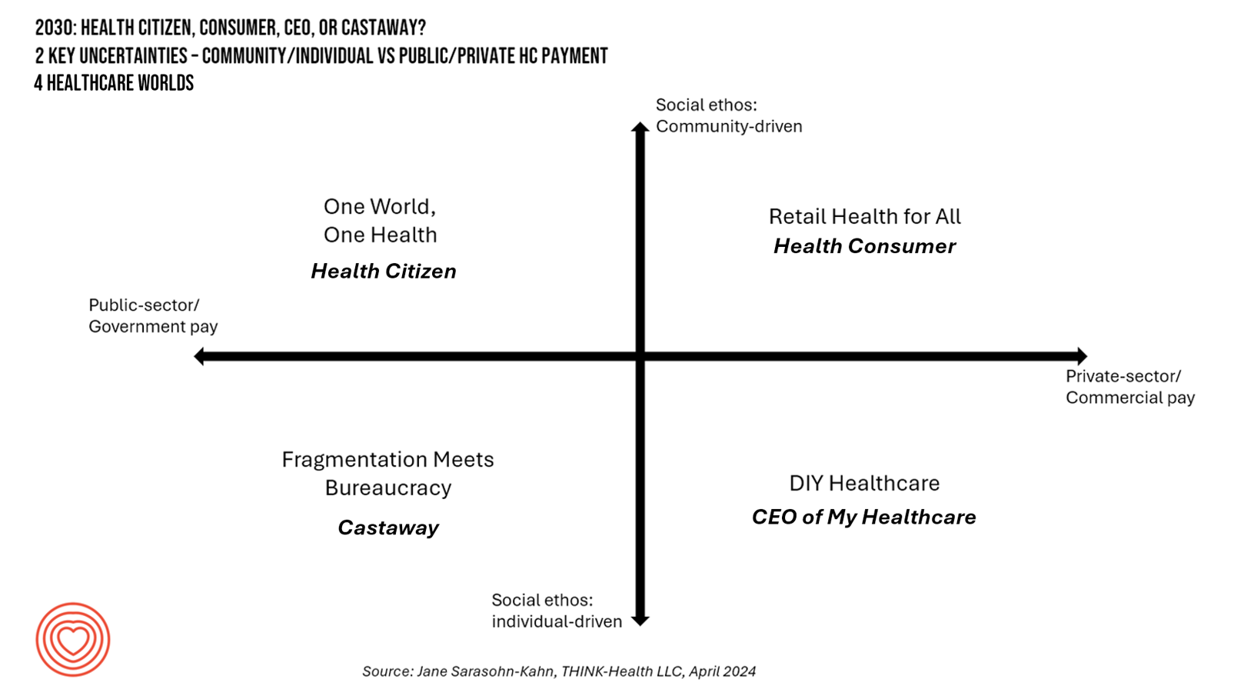
In the past few years, what event or innovation has had the metaphorical impact of hitting you upside the head and disrupted your best-laid plans in health care? A few such forces for me have been the COVID-19 pandemic, the emergence of Chat-GPT, and Russia’s invasion of Ukraine. That’s just three, and to be sure, there are several others that have compelled me to shift my mind-set about what I thought I knew-I-knew for my work with organizations spanning the health care ecosystem. I’m a long-time practitioner of scenario planning, thanks to the early education at the side of Ian
From Evolution to Innovation, from Health Care to Health: How Health Plans With Collaborators Are Re-Defining the Industry
As a constant observer and advisor across the health/care ecosystem, for me the concept of a “health plan” in the U.S. is getting fuzzier by the day. Furthermore, health plan members now see themselves as medical bill payers, seeking value and consumer-level services for their health insurance premium investment. Weaving these ideas together is my mission in preparing a session to deliver at the upcoming AHIP 2024 conference in June, I’m thinking a lot about the evolving nature of health insurance, plans, and the organizations that provide them. To help me define first principles, I turned to the American father
Accenture’s Great Expectations for a Decade of Deconstruction – the 2024 Life Trends Forecast
In the company’s 17th annual look into consumers’ “life trends,” Accenture finds that, top-line, “The harmony between people, tech and business is showing tensions, and society is in flux.” And these consumer-facing trends will also shape peoples’ attitudes about their health care, how they access and pay for it, and what kinds of services and support health consumers will expect in this era of “deconstruction.” Taken together, the trends noted in Accenture’s 2024 report on Life Trends finds that one-half of consumers, globally, are changing their life goals, making their jobs and retirement stability more important than
What If We Built a Consumer-Enchanting Health System in the Context of HLTH 2023? Building Blocks for the Scenario

What if….you were given the opportunity to build a health system from scratch in this new era of platforms, cloud computing, AI and machine learning, curious-digital-empowered consumers, and collaborators in retail and community settings operating close to peoples’ homes and workplaces? With the HLTH 2023 Conference meeting up in Vegas these past couple of days, this “what if” scenario can be constructed with announcements coming out of the meeting, coupled with recent developments in the larger health/care ecosystem. Start with General Catalyst’s news of engaging Dr. Marc Harrison, most recently CEO of Intermountain Health,
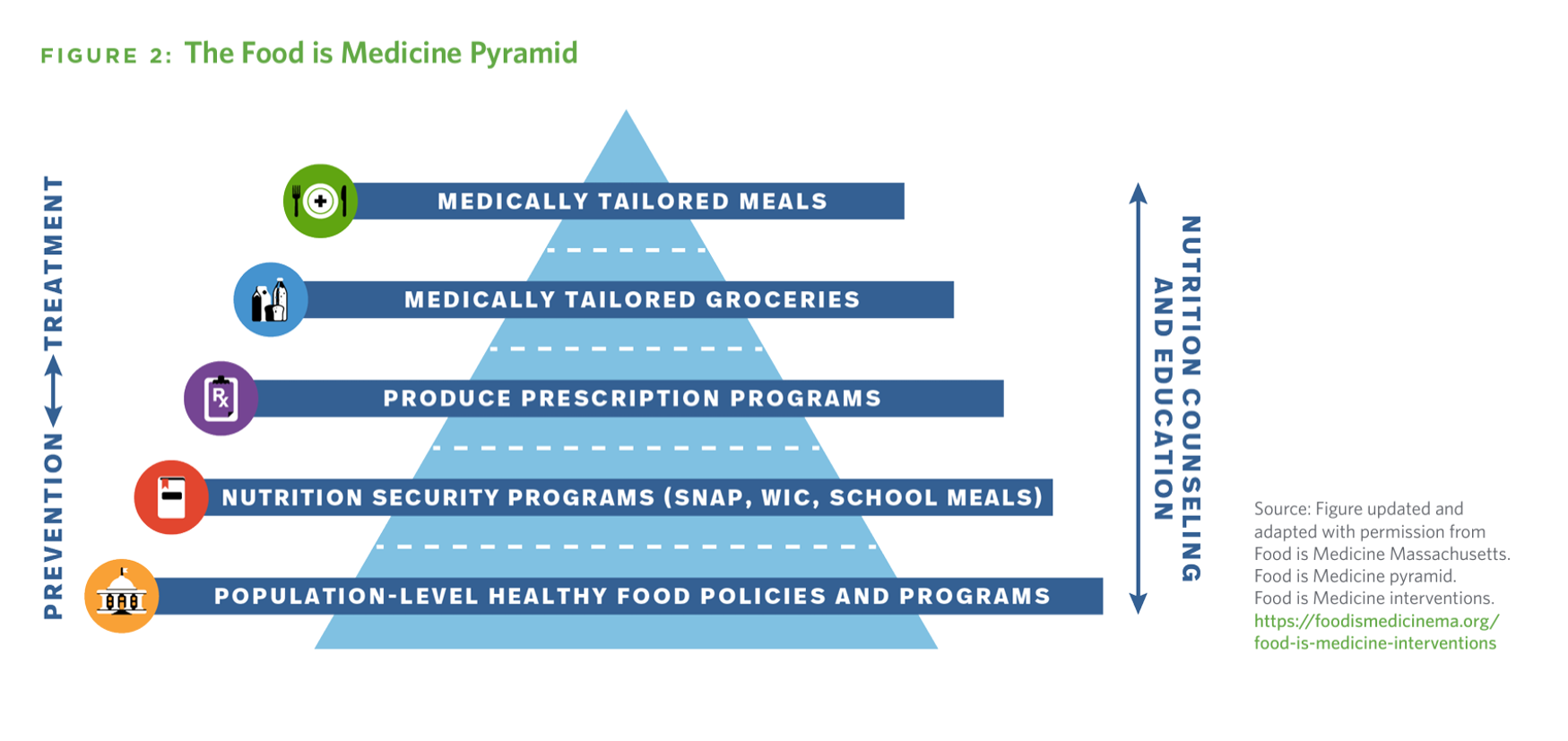
Food-As-Medicine Grows Its Cred Across the Health/Care and Retail Ecosystem
In the nation’s search for spending smarter on health care, the U.S. could save at least $13 billion a year through deploying medically-tailored meals for people enrolled in Medicare, Medicaid, and private insurance programs, according to the True Cost of Food, research published by the Tufts School of Nutrition Science and Policy collaborating with The Rockefeller Foundation. It’s been one year since the White House convened the Conference on Hunger, Nutrition, and Health, kicking off the Biden Administration’s national strategy to improve health citizens’ access to healthy food as a matter of public health and economic security.
Large Employers Expect More Employees Will Experience Prolonged Health Impacts Due to COVID-19. and a Note About Telehealth Engagement
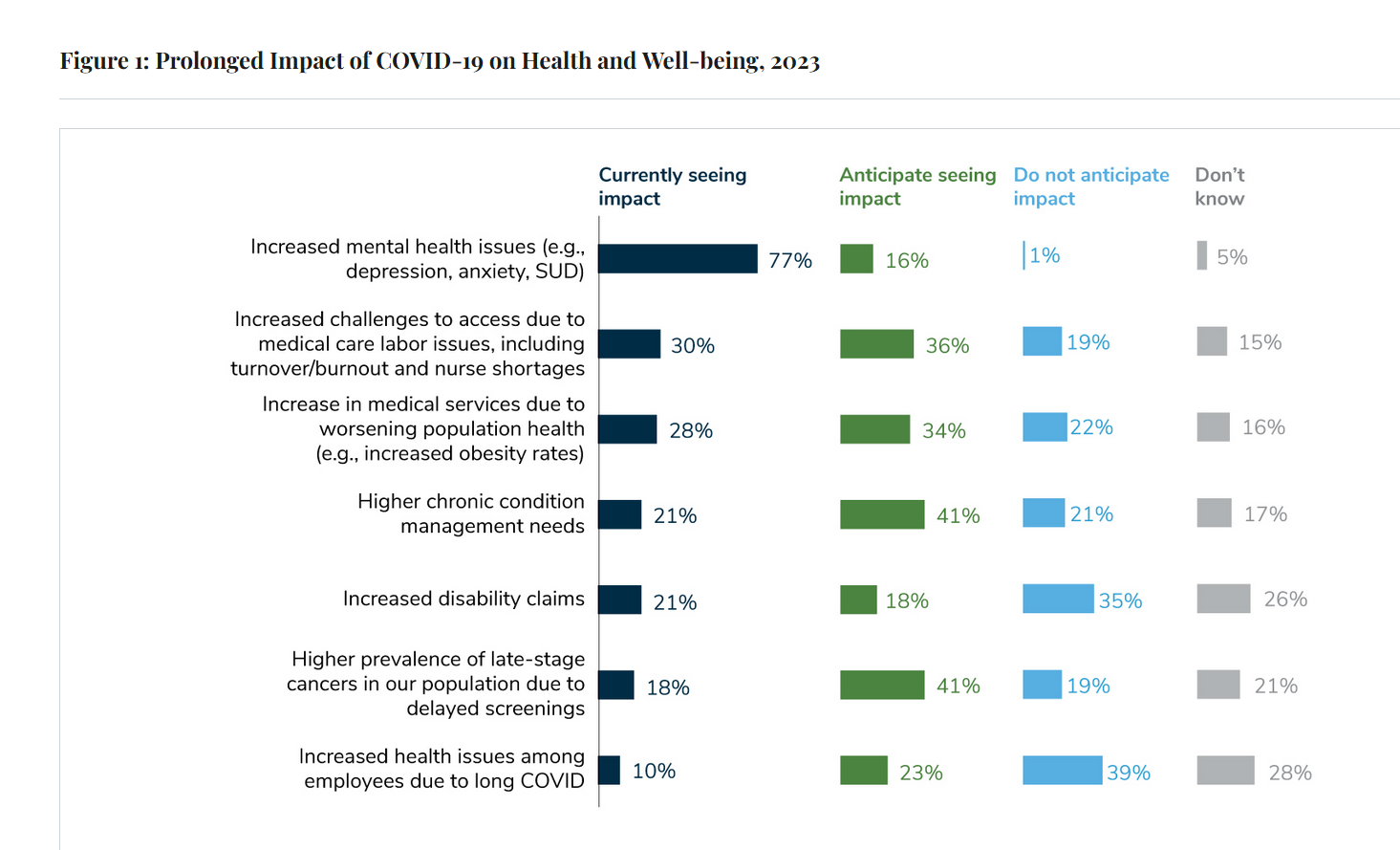
Due to their delayed return to medical services and diagnostic testing in the COVID-19 pandemic era, U.S. employees are expected to sustain serious health impacts that will drive employers’ health care costs, envisioned in the 2024 Large Employer Health Care Strategy Survey from the Business Group on Health (BGH). Dealing with mental health issues is the top health and well-being impact workers in large companies are addressing in 2023. Looking forward, large employers foresee their workers will be seeking care for chronic conditions and later-stage cancers that are diagnosed due to delayed screenings.
Cost Trumps Quality of Health Care for Consumers As Their Experience Has Eroded
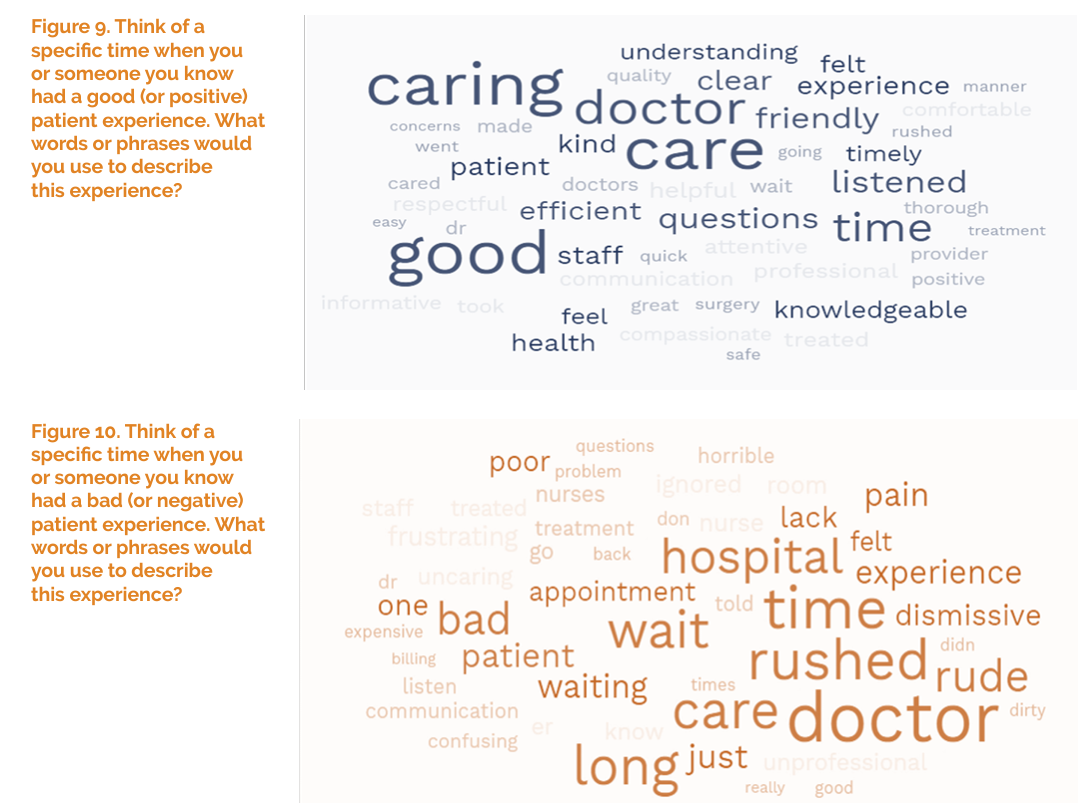
Patients’ perceptions of health care quality and experience have fallen in the three years since 2020, based on a July 2023 update from The Beryl Institute – Ipsos Px Pulse study. Start with health care quality, which 58% of U.S. adult patients ranked as “very good or good” in June 2020. The percent of health consumers evaluating their healthcare quality as very good or good fell to 41% of people in June 2023, an erosion of 17 percentage points, shown in the first chart. Next, consider patients’ ratings on their care experience,
Retail Clinics’ Growing Role in Health Care and Prescription Drug Sales
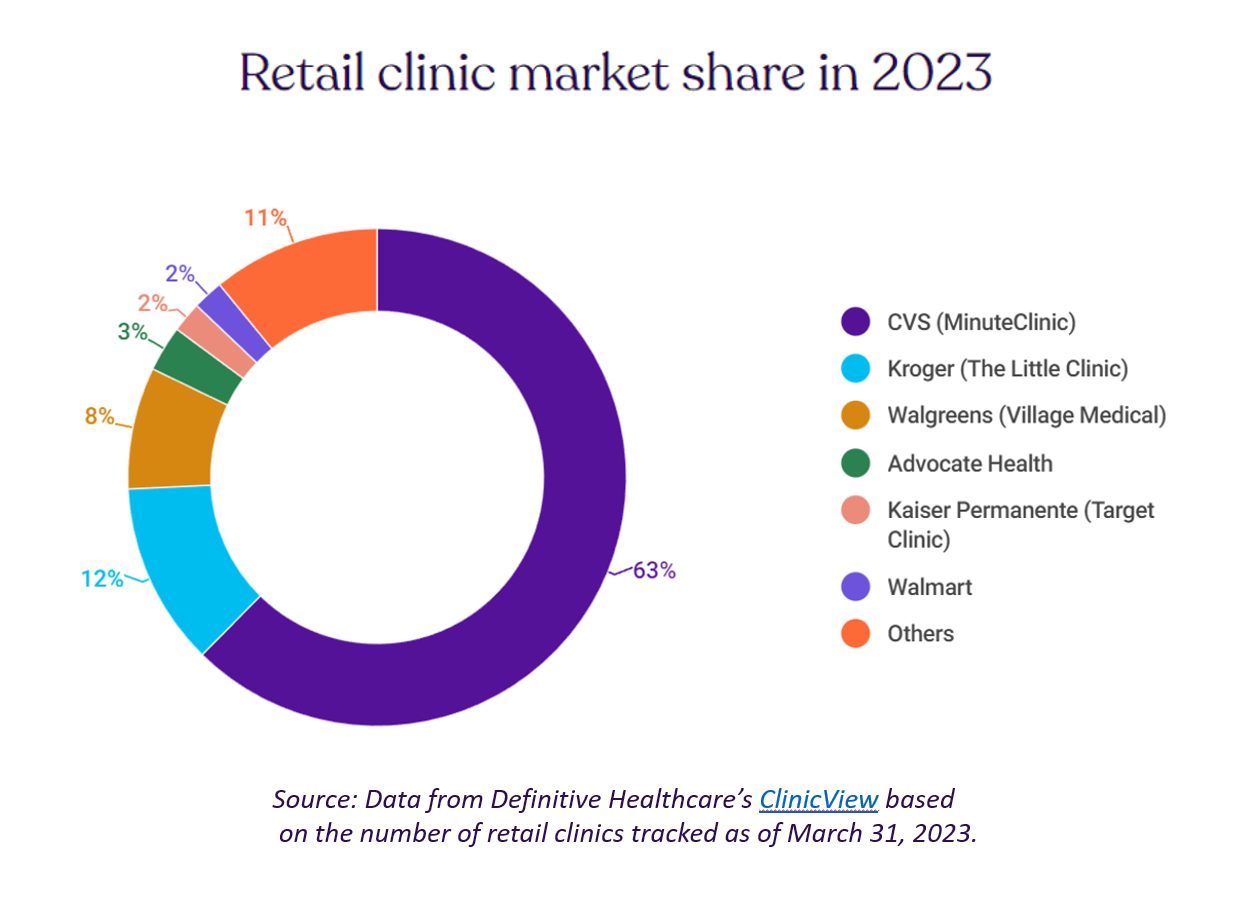
“It seemed like an odd pairing: shampoo and a throat swab,” observes a new report on the growth of retail health from Definitive Healthcare. But retail clinics are no longer, as the paper explains, “an experiment of a few grocery stores….they’re becoming a major force in the U.S. healthcare system,” asserts the thesis of Retailers in healthcare: A catalyst for provider evolution. While the use of emergency departments fell by 1% in the past five years, the use of retail clinics expanded by 70%, Definitive Healthcare calculated. Most retail clinics are owned by
A Public Health Wake-Up Call: Reading Between the Lines in IQVIA’s 2023 Use of Medicines Report
Reviewing the annual 2023 report from the IQVIA Institute for Human Data Science discussing The Use of Medicines in the U.S. is always a detailed, deep, and insightful dive into the state of prescription drugs. It’s a volume speaking volumes on the current picture of prescribed meds, spending and revenues, health care utilization trends, and a forecast looking out to 2027. In my read of this year’s review, I see a flashing light for U.S. health care: “Wake up, public health!” I’ve pulled out a few of the data points that speak to me about population health, prevention and early
The New Deaths of Despair in America – Among U.S. Children
The phenomenon of Deaths of Despair is the short-hand name for rising mortality among certainly people living in the U.S. due to overdose, accidents, and suicide. Angus Deaton and Anne Case published their first of many research papers on Deaths of Despair in 2015. Their research uncovered the risks of dying a Death of Despair to be higher among men, especially those between the ages of 25 and 64. But mortality isn’t only going in the wrong direction for those people most closely associated with the Deaths of Despair demographic: there’s another life-span line graph moving in the wrong direction,
What Are Patients Looking for in a Doctor? It Depends on Who You Ask…and Their Race
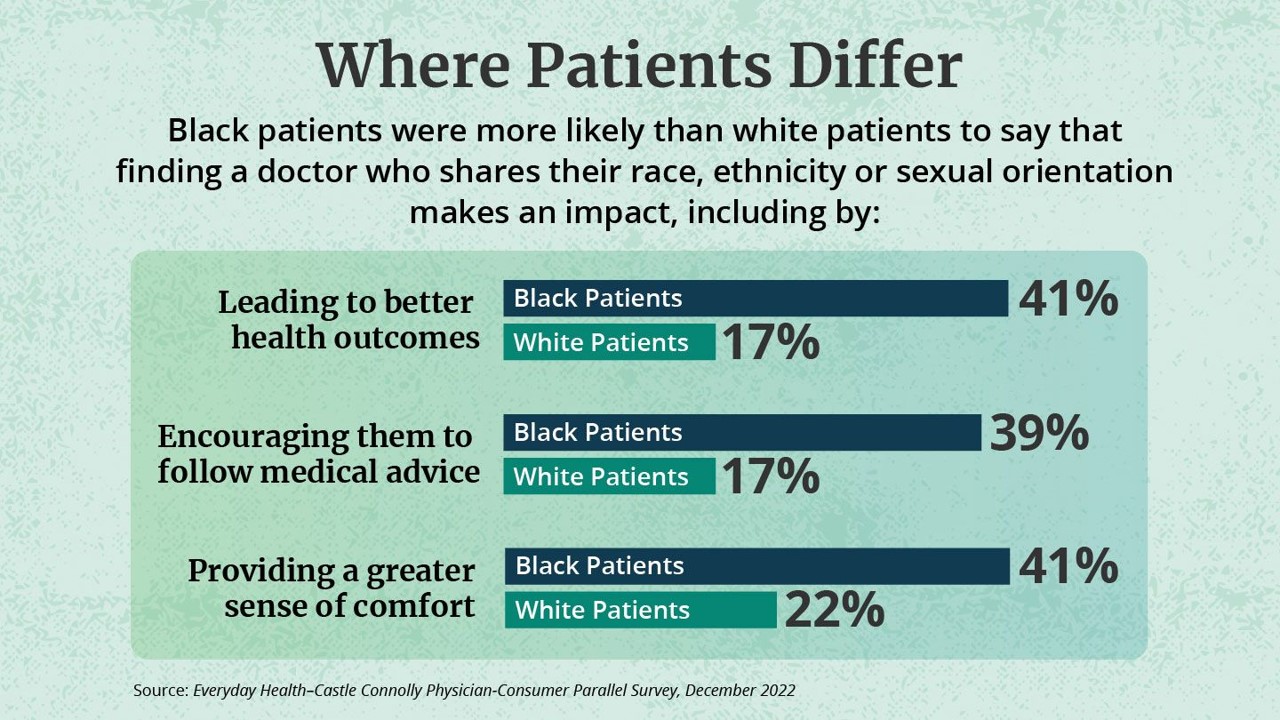
While the same proportion of Black and White patients say they are looking for a doctor with empathy and compassion, there are relatively large differences between patients based on their race, found in the Everyday Health-Castle Connolly Physician-Consumer study. The survey was conducted in December 2022 among a group of 1,001 U.S. consumers and 277 Castle Connolly health care professionals. As the first bar chart illustrates “where patients differ, “Black people were nearly twice as likely as white people (41 percent versus 22 percent) to completely agree that they would be more comfortable and
Your Grocery Store as Health/Care Destination: Welcome Kroger to the Clinical Trials Community

Our grocery stores were essential touchpoints for us during the COVID-19 lockdown era and thereafter, addressing our basic needs for food and medicines and even social health from early 2020 and since. Grocery stores have been morphing into health/care destinations for the past decade, in the best cases bolstering nutrition, supporting medication adherence and patient outcomes, and helping us curate healthy grocery carts with nutritionists as part of the store pharmacy team. Now Kroger continues to expand its health/care footprint and capabilities, becoming a clinical trials channel as announced in its January 24th press
Digital Health Funding Updates from FINN + Galen and Silicon Valley Bank – Context for JPM2023
As we enter the week’s brainstorms and deal-making prospects this week at the annual JP Morgan meet-up for healthcare, I’m kicking off Health Populi’s posts this week by diving into two major reports published in sync with this meeting that’s so pivotal and important for the digital health community: the Silicon Valley Bank (SVB) 2022 Annual Report on Healthcare Investments and Exits and the 2022 Global State of Digital Health Report from FINN Partners and Galen Growth SVB notes that venture funding in healthcare fell in terms of both deals and dollars each quarter
The Heart Health Continuum at #CES2023 – From Prevention and Monitoring to Healthy Eating and Sleep
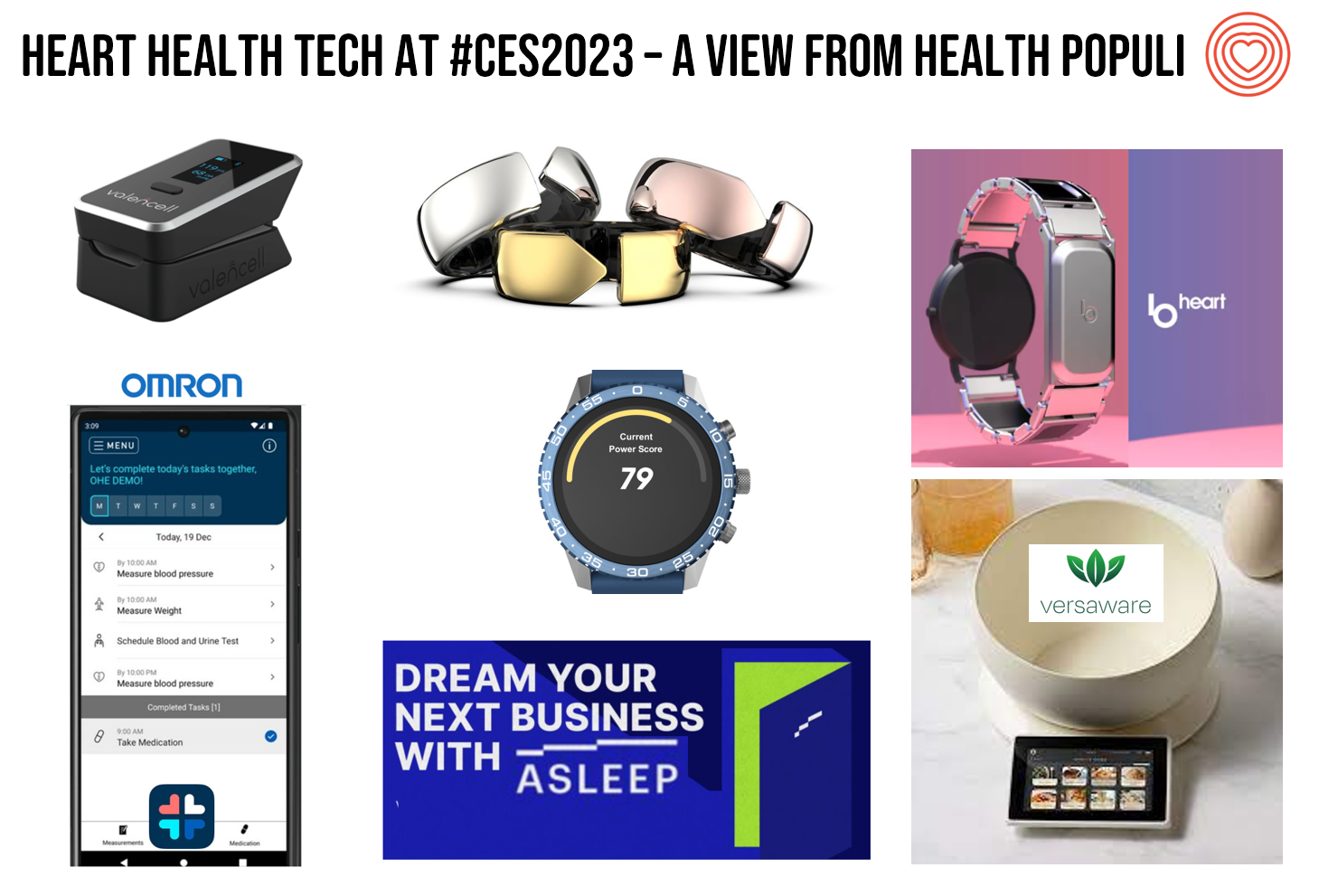
“Are we losing the battle against heart disease?” asks the lead article featured in the January 2023 issue of the AARP Bulletin. “Despite breathtaking medical advancements since President Harry Truman declared war on heart disease 75 years ago, researchers have observed a disturbing trend that started in 2009: America’s death rate from heart-related conditions is climbing again,” the detailed essay explains. AARP is in fact a very visible stakeholder in the 2023 CES, collaborating on the AgeTech content track at the tech conference. The track covers all aspects of aging well, from financial health to entertainment,
In Search of Clinical Effectiveness, But “Investment Exuberance?” Not So Much. Insights From FINN Partners and Galen Growth at HLTH 2022

While venture funding for digital health technology declined globally by 35% in the first three quarters of 2022 compared with 2021, this marks a “return to normal” based on the assessment in the Global State of Digital Health Report from FINN Partners and Galen Growth, published today and launched during the HLTH 2022 conference. The report analyzes data from over 12,000 digital health ventures tracked by Galen Growth’s HealthTech Alpha platform. The first chart illustrates the change in venture funding by therapeutic area, showing downturns in four of the five areas called
The Direct Link Between Value-Based Health Care, Digital Transformation and Social Determinants – Insights from Innovaccer and Morning Consult
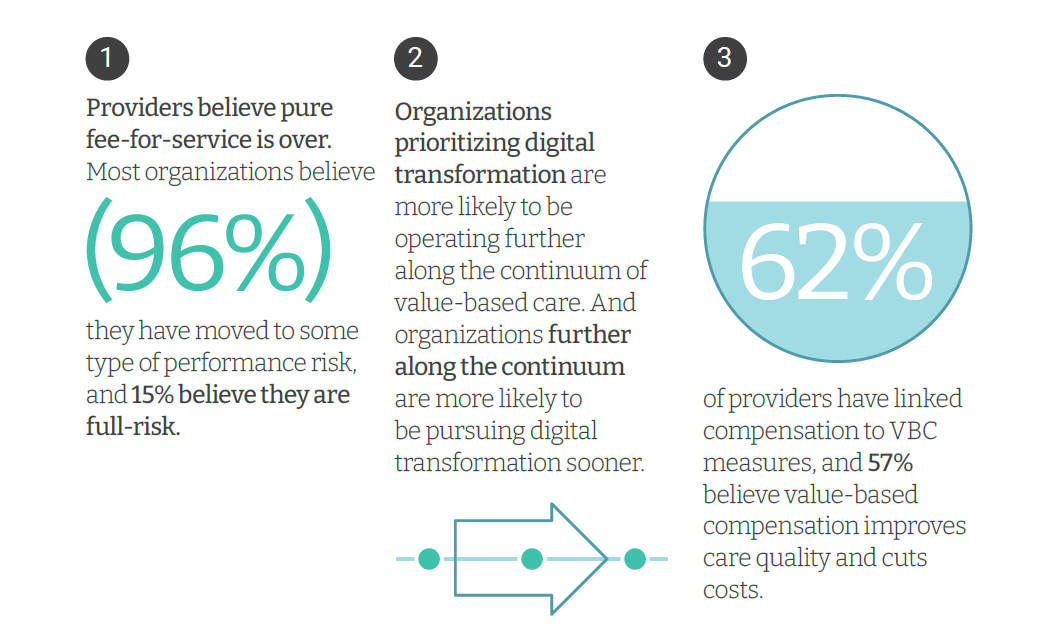
Only 4% of health care payments in the U.S. are pure fee-for-service (FFS) these days. “The end of pure FFS is near,” according to The State and Science of Value-Based Care, a report-out of survey research from Innovaccer and Morning Consult. Innovaccer, a health cloud/data analytics company, worked with Morning Consult to do deep-dive interviews with 75 senior health care executives; research was conducted in November and December 2021, so these perspectives represent those of health system leaders at the start of 2022. The full report is worth your read; my focus in this Health
Partnering Up in the Health Care Ecosystem to Drive Transformation – for Organizations and Health Consumers Alike
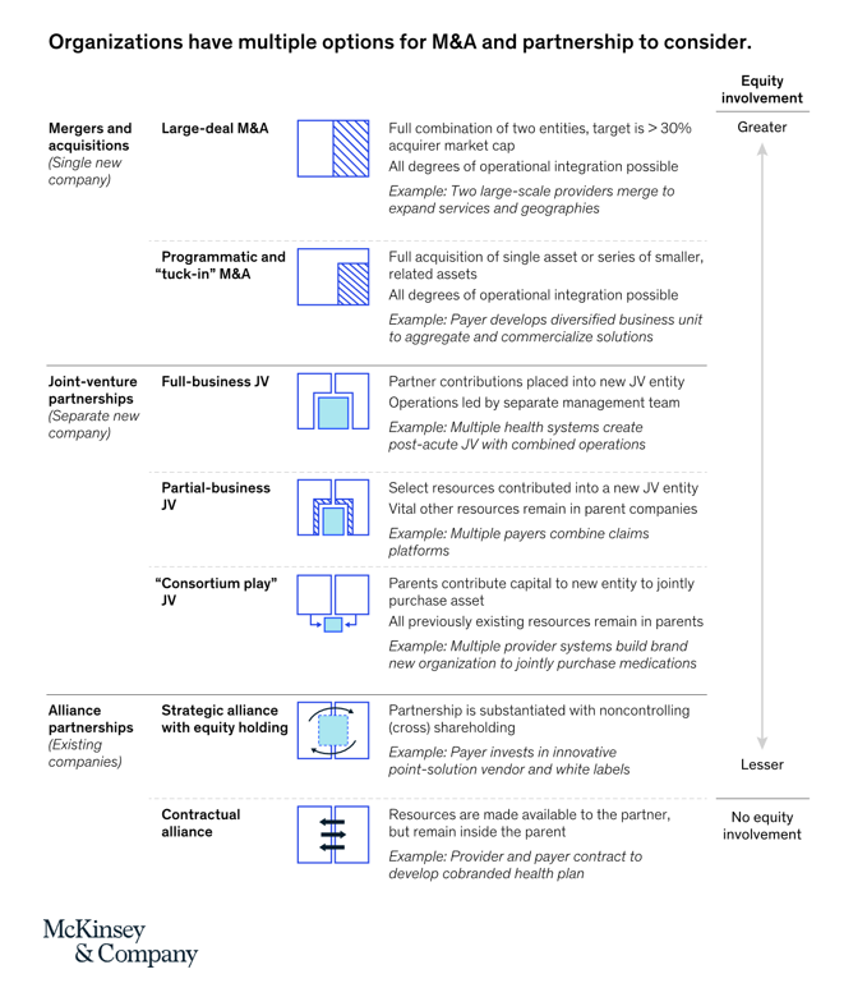
“Partnerships, including JVs and alliances with other healthcare organizations and with new entrants, are just one way to access new capabilities, unlock speed to market, and achieve capital, scale, and operational efficiencies” in health care transformations. “In an environment with continued competition for attractive assets and significant capital in play from institutional investors, these partnerships may also be the most accessible way for organizations to capture value in expanding healthcare services and technology value pools,” we learn in Overcoming the cost of healthcare transformation through partnerships from a team of health care folks with McKinsey & Company.
Your State as a Determinant of Health: Sharecare’s 2021 Community Well-Being Index
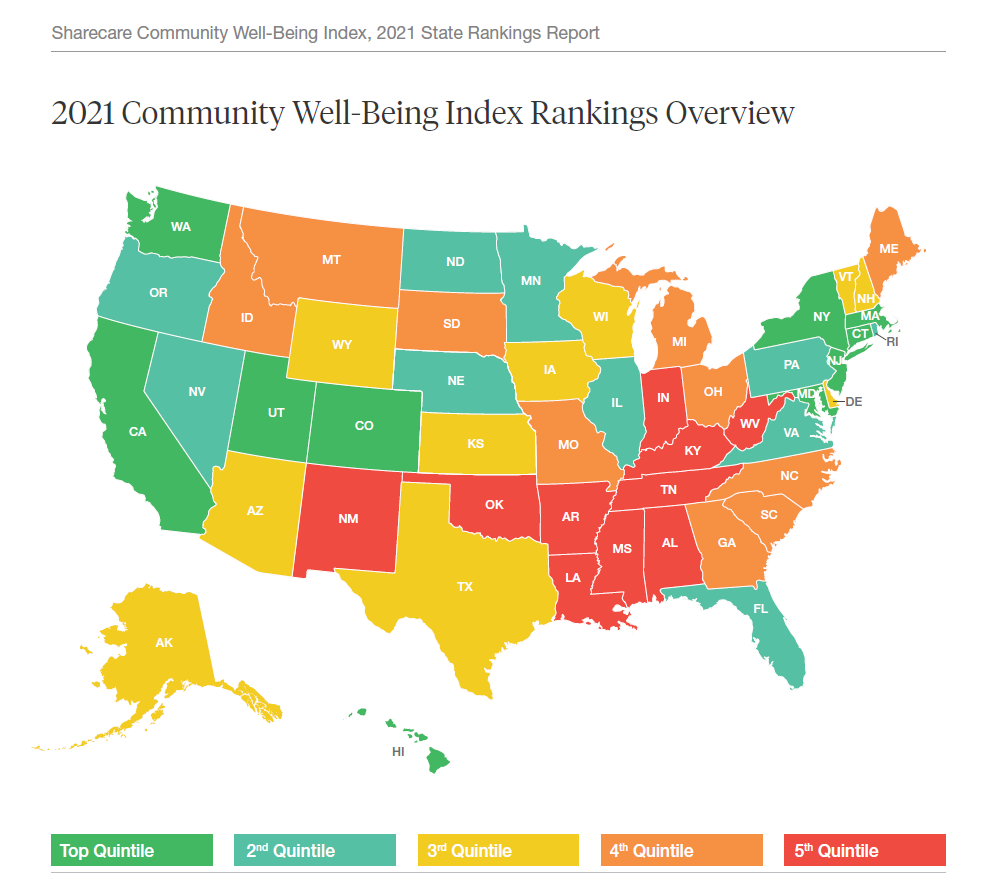
People whose sense of well-being shifted positively in the past two years are finding greater personal purpose and financial health, we see in Sharecare’s Community Well-Being Index – 2021 State Rankings Report. Sharecare has been annually tracking well-being across the 50 U.S. states since 2008. When the study launched, Well-Being Index evaluated five domains: physical, social, community, purpose, and financial. In 2020, Sharecare began a collaboration with the Boston University School of Public Health to expand the Index, including drivers of health such as, Healthcare access (like physician supply per 1,000
Use of Preventive Health Services Declined Among Commercially Insured People – With Big Differences in Telehealth for Non-White People, Castlight Finds
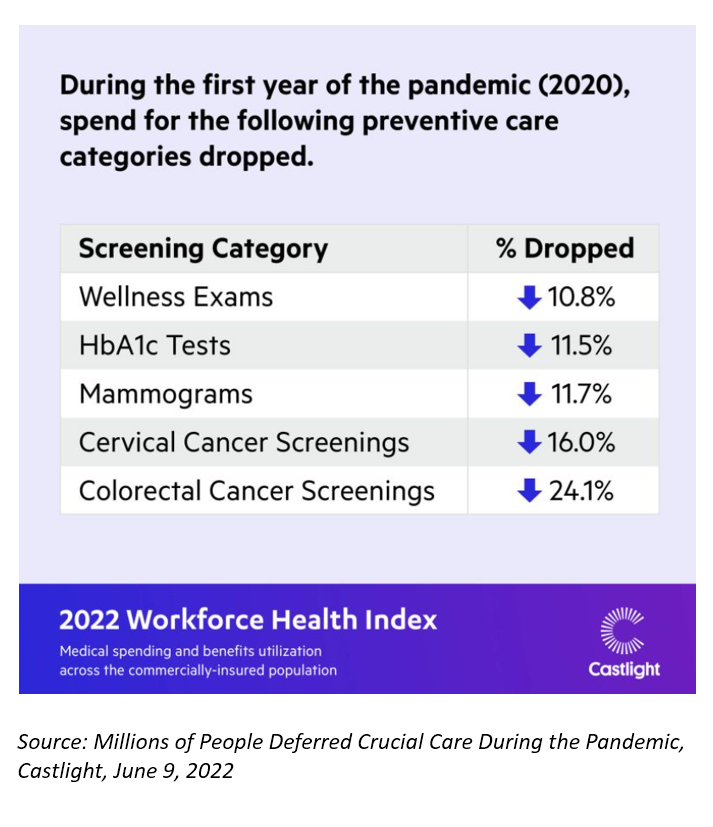
Declines in preventive care services like cancer screenings and blood glucose testing concern employers, whose continued to cover health insurance for employees during the pandemic. “As we enter the third year of the COVID-19 pandemic, employers continue to battle escalating clinical issues, including delayed care for chronic conditions, postponed preventive screenings, and the exponential increase in demand for behavioral health services,” the Chief Medical Officer for Castlight Health notes in an analysis of medical claims titled Millions of People Deferred Crucial Care During the Pandemic, published in June. The
The 2022 US Health System Report Card: Pretty Terrific If You Live in Hawaii or Massachusetts
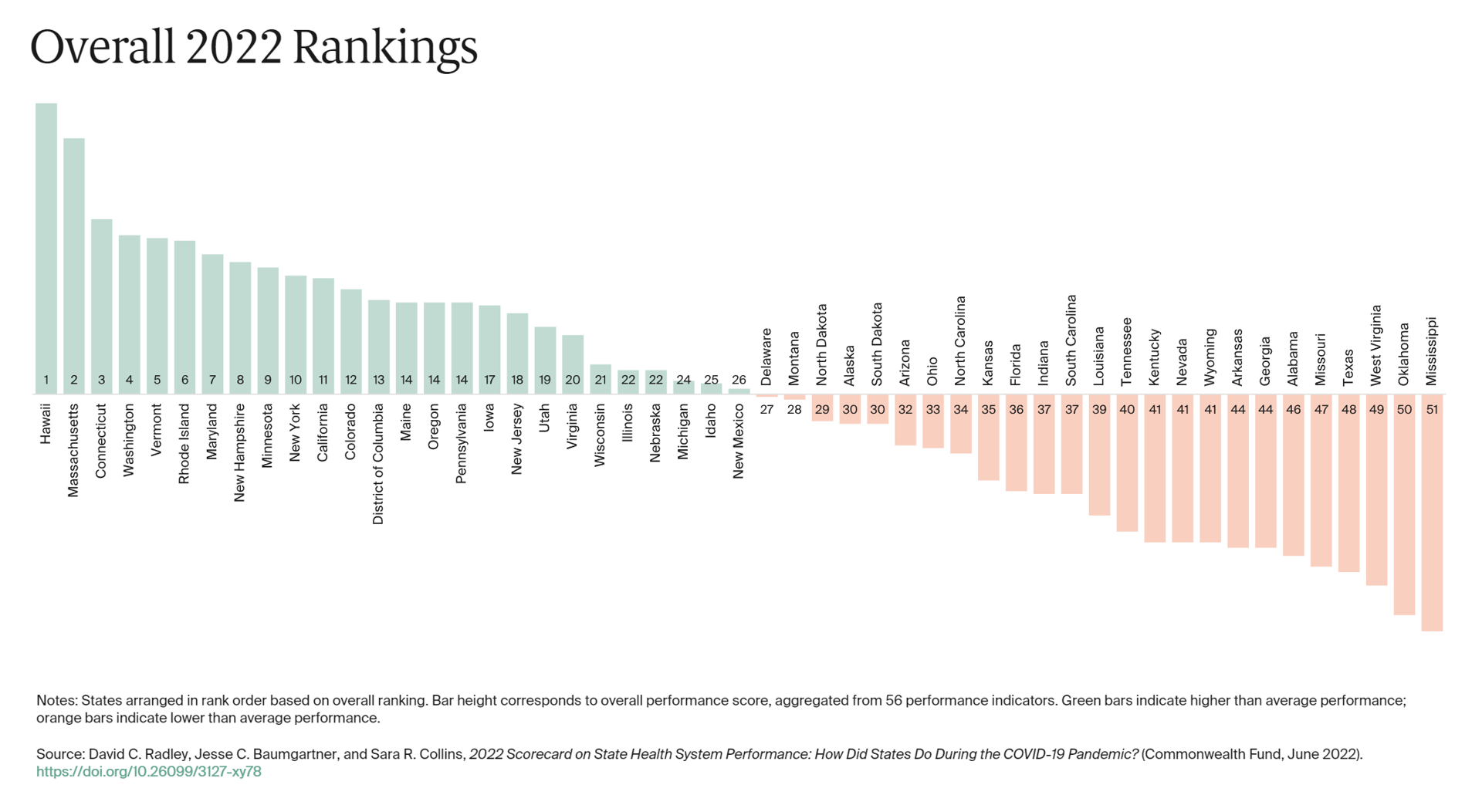
The best U.S. states to live in for health and health care are Hawaii, Massachusetts, Connecticut, Washington, Vermont, Rhode Island, and Maryland… Those are the top health system rankings in the new 2022 Scorecard on State Health System Performance annual report from the Commonwealth Fund. If you live in Mississippi, Oklahoma, West Virginia, Texas, Missouri, Alabama, Georgia, or Arkansas, your health care and outcomes are less likely to be top-notch, the Fund’s research concluded. The Commonwealth Fund has conducted this study since 2006, assessing a range
The Color of Care – Oprah and The Smithsonian Channel Partner on Health Equity
A new documentary and educational campaign on health equity will be launched on May 1st, 2022, from Oprah’s Harpo Productions studio partnering with The Smithsonian Channel. The Color of Care documents stories of people who have lost loved ones in the COVID-19 pandemic as well as expert interviews with frontline workers and public health experts and researchers sharing data on systemic racism in health care that has underpinned racial health disparities since slavery was instituted in America. Oprah’s website talked about the project, quoting her saying, “At the height of the pandemic, I read something that stopped me in
How Business Can Bolster Determinants of Health: The Marmot Review for Industry
“Until now, focus on….the social determinants of health has been for government and civil society. The private sector has not been involved in the discussion or, worse, has been seen as part of the problem. It is time this changed,” asserts the report, The Business of Health Equity: The Marmot Review for Industry, sponsored by Legal & General in collaboration with University College London (UCL) Institute of Health Equity, led by Sir Michael Marmot. Sir Michael has been researching and writing about social determinants of health and health equity for decades, culminating publications
Techquity: How Technology Can Help to Scale Health and Digital Equity, Live from VIVE 2022
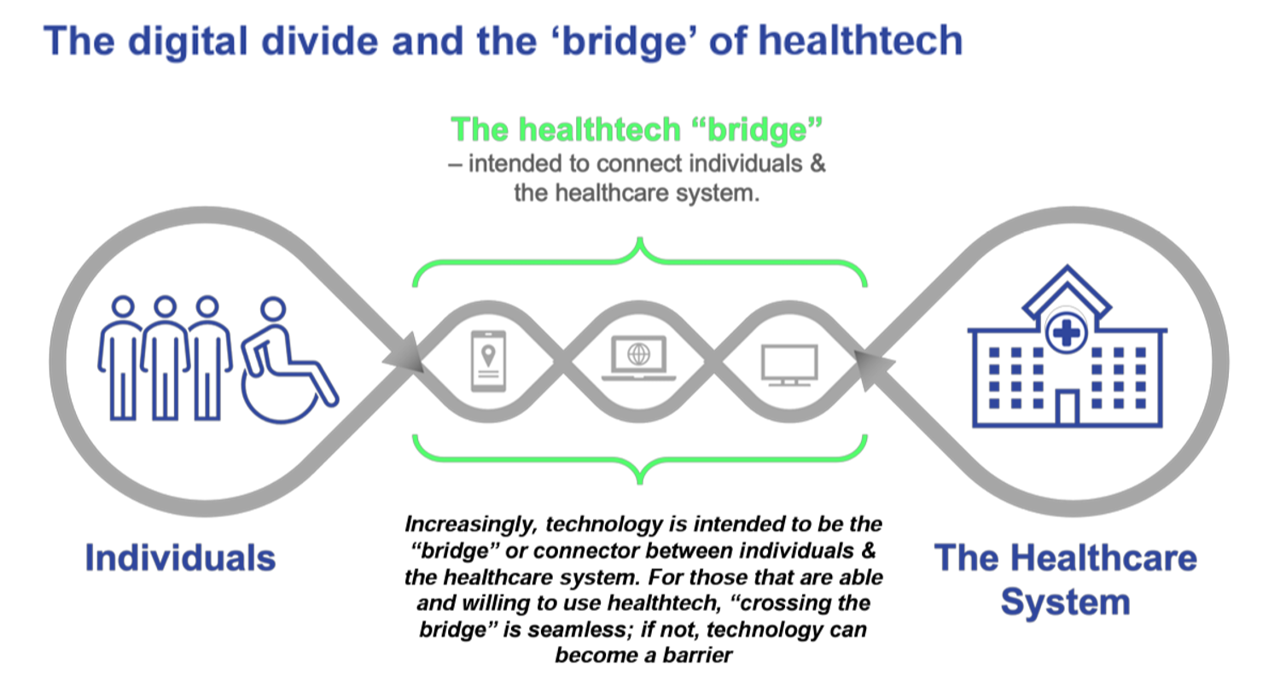
The COVID-19 pandemic revealed long-systemic health disparities in the U.S. and in other parts of the world. Income inequality, sickly environments in homes and communities (think unclean air and water), lack of public transportation and nutritious food deserts combine to limit peoples’ health and well-being., Beyond the traditional social determinants of health, such as these, we’ve called out another health risk that became crucial for life in the coronavirus pandemic era: digital connectivity, Indeed, WiFi and broadband represent the newest social determinant of health to add to a growing list of risk factors that challenge health citizens’ health. Kudos to
Designing Digital Health for Public Health Preparedness and Equity: the Consumer Tech Association Doubles Down
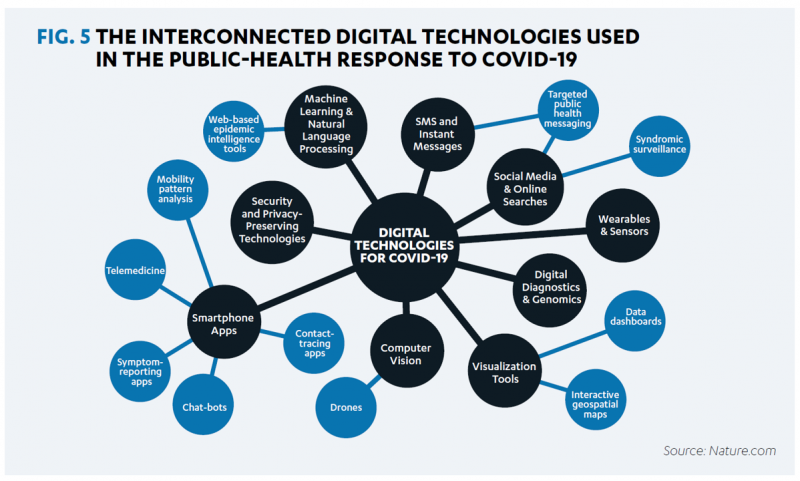
A coalition of health care providers, health plans, technology innovators, NGOs, and medical societies has come together as the Public Health Tech Initiative (PHTI), endorsed by the Consumer Technology Association (CTA) with the goal of advancing the use of trustworthy digital health to proactively meet the challenge of future public health emergencies….like pandemics. At the same time, CTA has published a paper on Advancing Health Equity Through Technology which complements and reinforces the PHTI announcement and objective. The paper that details the PHTI program, Using Heath Technology to Response to Public Health Emergencies, identifies the two focus areas: Digital health
Health Disparities in America: JAMA Talks Structural Racism in U.S. Health Care

“Racial and ethnic inequities in the US health care system have been unremitting since the beginning of the country. In the 19th and 20th centuries, segregated black hospitals were emblematic of separate but unequal health care,” begins the editorial introducing an entire issue of JAMA dedicated to racial and ethnic disparities and inequities in medicine and health care, published August 17, 2021. This is not your typical edition of the Journal of the American Medical Association. The coronavirus pandemic has changed so many aspects of American health care for so many people, including doctors. Since the second quarter of 2020,
Can the U.S. Improve Health System Performance with Digital Health Tools? Pondering A Big Question for #HIMSS21
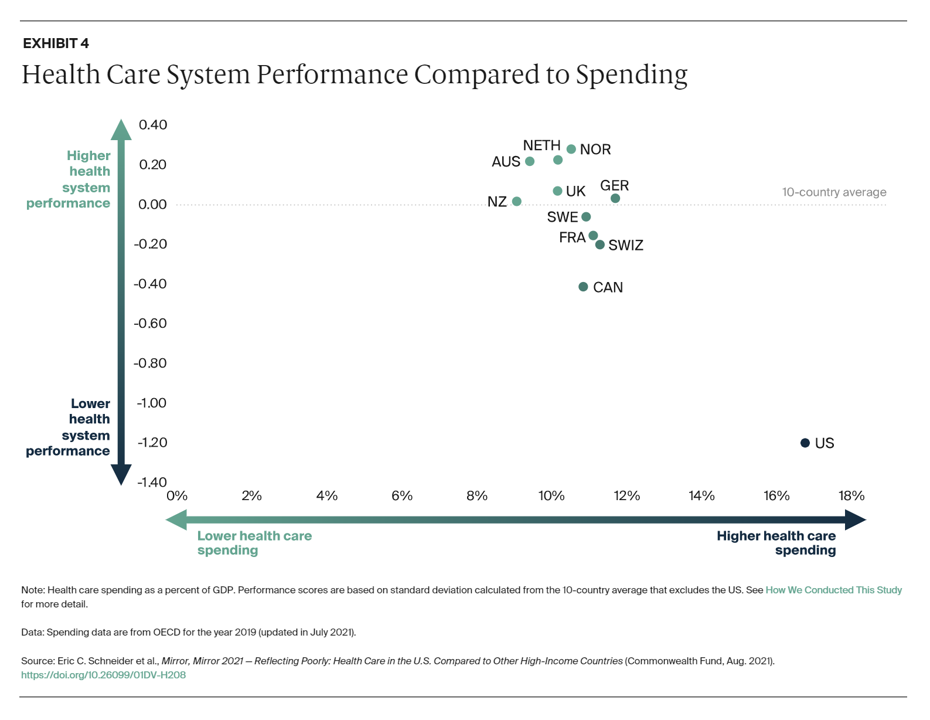
Simply put, is the equation, “Spend more, get less” a sustainable business model? Of course not. But that’s the simple math on U.S. health care spending and what comes from it, according to Mirror, Mirror 2021: Reflecting Poorly, a perennial report from The Commonwealth Fund that compares health system performance across eleven developed countries. The first table details the metrics that the Fund compares across the eleven peer nations, which included Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States. The metrics compared were access to care, care process, administrative efficiency, equity,
Women’s Health Re-shaped by COVID-19
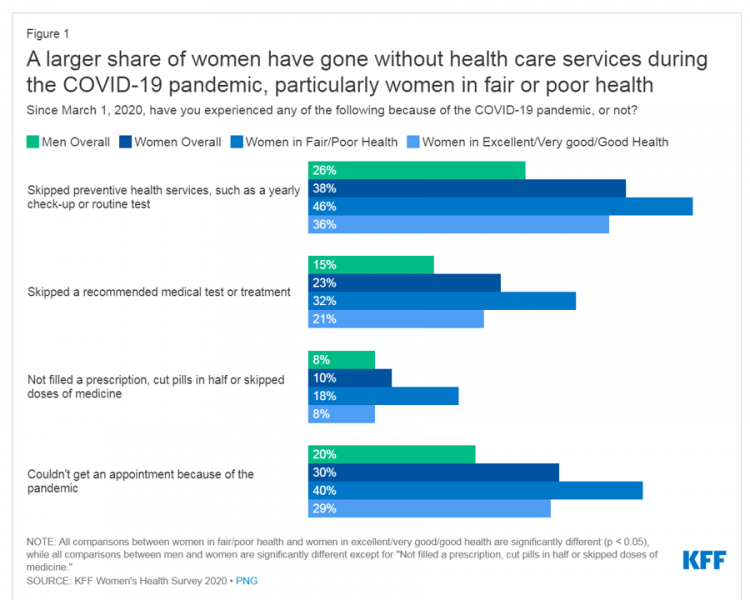
While women continue to outlive men in the U.S. in terms of life expectancy, the COVID-19 pandemic revealed continued healthcare access, physical and mental health disparities, and economic inequities for women in America. I addressed the changing state of post-pandemic women’s health in my latest contribution to the Medecision Liberation blog. This first graphic illustrates how women interacted with the U.S. health system during the pandemic in 2020. These data come from Kaiser Family Foundation’s women’s health survey conducted from the beginning of the pandemic starting March 1, 2020, and discovered that women in poorer or fair more likely went
Eli Lilly Bets on U.S. Well-Being at the Olympics
The U.S. Olympic team will be competing in Tokyo for first-place medals across many athletic events, each nation’s most physically-fit citizens going for gold. When it comes to the U.S. ranking on the world roster of population health outcomes, American ranks low on many key metrics, especially given that the U.S. does rank #1 in one key stat: healthcare spending. Reminding us of America’s lowly-placed health outcomes, the Eli Lilly Company is collaborating with Team USA, the US Olympic and Paralympic teams, to promote “Our Collective Health” with the message that, “Watching the success of our athletes will once again
The Healthcare and Macro-Economic Impacts of Living with Endemic COVID – Listening to Fitch
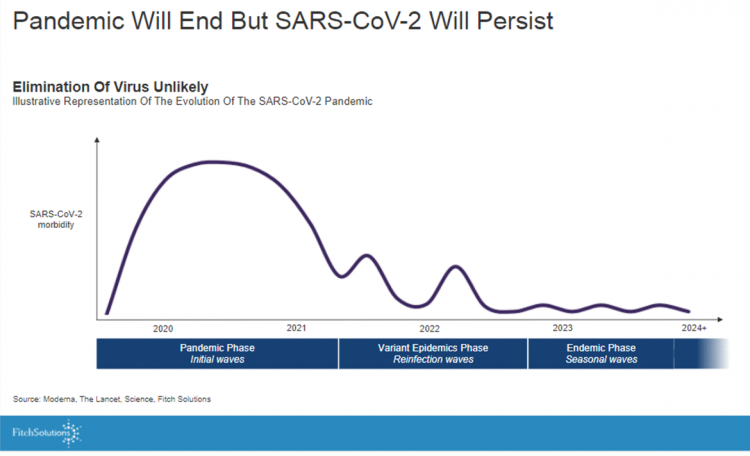
Getting totally rid of the coronavirus isn’t likely, so we humans must accept the fact that SARS-CoV-2 will be endemic. The economic and healthcare system impacts of this were explored in the Post-Covid Healthcare Landscape, delivered by Fitch Solutions’ Jamie Davies and Beau Noafshar, leaders in the Pharmaceuticals, Healthcare, and Medical Devices groups. I welcomed the opportunity to learn from this team’s approach in weaving together the dynamic issues that help us to plan for the long-tail of COVID-19 and its impact on the economy and prospects for the health care industry and health citizens. The first graph illustrates the
Post-Pandemic, U.S. Healthcare is Entering a “Provide More Care For Less” Era – Pondering PwC’s 2022 Forecast

In the COVID-19 pandemic, health care spending in the U.S. increased by a relatively low 6.0% in 2020. This year, medical cost trend will rise by 7.0%, expected to decline a bit in 2022 according to the annual study from PwC Health Research Institute, Medical Cost Trend: Behind the Numbers 2022. What’s “behind these numbers” are factors that will increase medical spending (the “inflators” in PwC speak) and the “deflators” that lower costs. Looking around the future corner, the inflators are expected to be: A COVID-19 “hangover,” leading to increased health care services utilization Preparations for the next pandemic, and
The ROI on Virtual Care – Thinking About Value and Future Prospects With the AMA
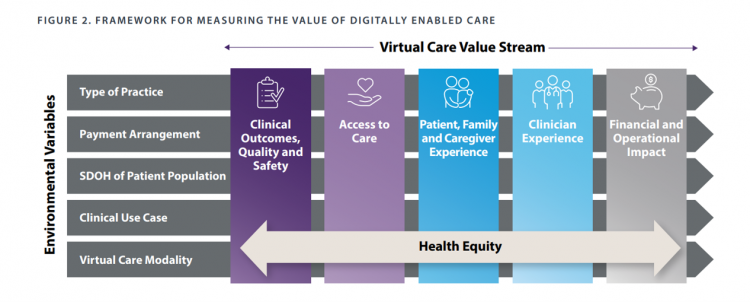
When a new technology or product starts to get used in a market, it follows a diffusion curve whose slope depends on the pace of adoption in that market. For telehealth, that S-curve has had a very long and fairly flat front-end of the “S” followed by a hockey stick trajectory in March and April 2020 as the COVID-19 pandemic was an exogenous shock to in-person health care delivery. The first chart from the CDC illustrates that dramatic growth in the use of telehealth ratcheting up since the first case of COVID-19 was diagnosed in the U.S. Virtual care has
Spending on Medicines In and Post-COVID Say a Lot About Patients and Larger Healthcare Trends – an IQVIA Update
Spending on medicines, globally, will rebound this year and rise above pre-pandemic levels through 2025. Between 2021 and 2025, the annual growth global growth rate for prescription drugs spending is expected to range from 3% to 6%, a $1.6 trillion bill for the worlds’s total Rx medicines market. That relatively low single-digit growth rate is tempered by savings from biosimilars and the loss of brand exclusivity (that is, more generics coming to market). On the faster-growth side, we can expect two big therapeutic areas to drive spending upward: oncology and immunology, projected to expand by 9% to 12% each year
How Fruits and Veg Can Make Health and Lower Costs – Calling Chef José Andrés to the White House
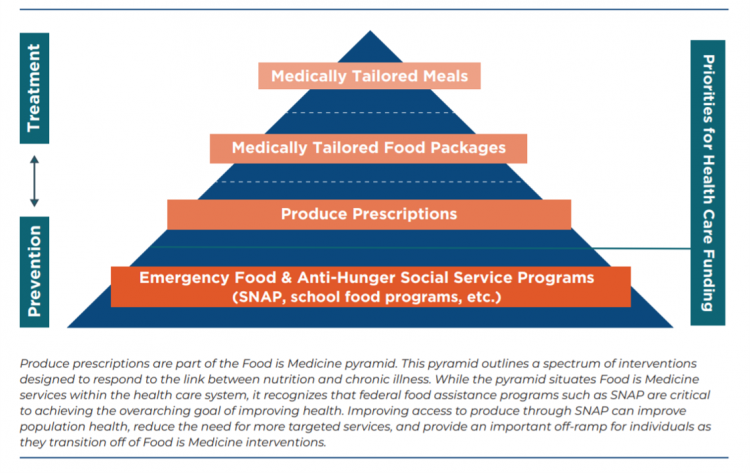
Springtime is finally emerging on the east coast of the U.S. and my local CSA farm is on my mind. It’s timely, then, to re-visit a research paper on subsidizing fruits and vegetables from a March 2019 issue of PLOS as an introduction to a new initiative growing out of The Center for Health Law and Policy Innovation of Harvard Law School (CHLPI) on produce prescriptions. Timely, too, that Chef José Andrés has been called to President Biden’s White House to help address food security in America. First, let’s look at the research in PLOS: Cost-effectiveness of financial incentives for
How to Restore Americans’ Confidence in U.S. Health Care: Deal With Access and Cost
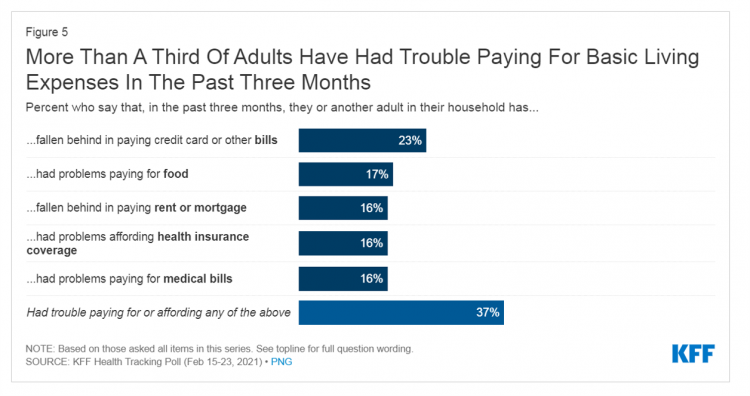
With a vaccine supply proliferating in the U.S. and more health citizens getting their first jabs, there’s growing optimism in America looking to the next-normal by, perhaps, July 4th holiday weekend as President Biden reads the pandemic tea leaves. But that won’t mean Americans will be ready to return to pre-pandemic health care visits to hospital and doctor’s offices. Now that hygiene protocols are well-established in health care providers’ settings, at least two other major consumer barriers to seeking care must be addressed: cost and access. The latest (March 2021) Kaiser Family Foundation Tracking Poll learned that at least one
Value-Based Health Care Needs All Stakeholders at the Table – Especially the Patient

2021 is the 20th anniversary of the University of Michigan Center for Value-Based Insurance Design (V-BID). On March 10th, V-BID held its annual Summit, celebrating the Center’s 20 years of innovation and scholarship. The Center is led by Dr. Mark Fendrick, and has an active and innovative advisory board. [Note: I may be biased as a University of Michigan graduate of both the School of Public Health and Rackham School of Graduate Studies in Economics]. Some of the most important areas of the Center’s impact include initiatives addressing low-value care, waste in U.S. health care, patient assistance programs, Medicare
Americans Lost Future Life-Years in 2020: How Much Life Was Lost Depends on the Color of One’s Skin
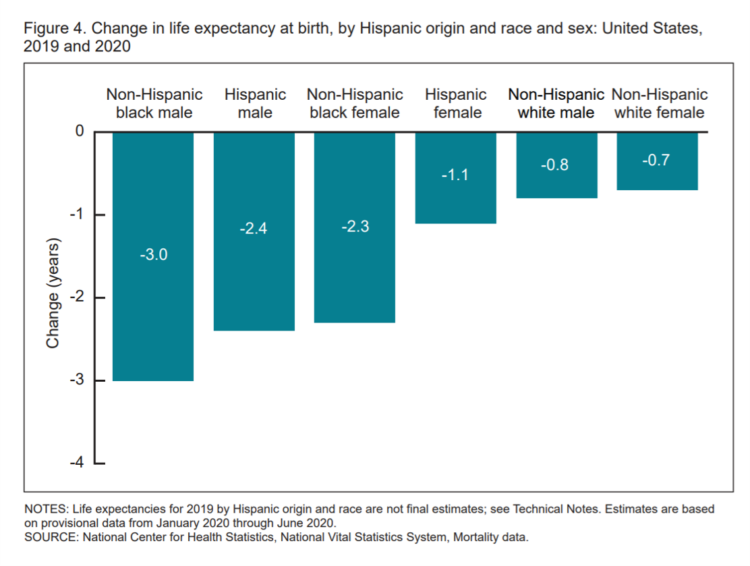
Some people remark about 2020 being a “lost year” in the wake of the coronavirus pandemic. That happens to be a true statement, sadly not in jest: in the U.S., life expectancy at birth fell by one full year over the first half of 2020 compared with 2019, to 77.8 years. In 2019, life expectancy at birth was 78.8 years, according to data shared by the National Center for Health Statistics (NCHS), part of the Centers for Disease Control and Prevention (CDC). Life expectancy at birth declined for both females and males, shown in the first chart. The differences between
Dr. Burnout – The 2021 Medscape Physician Burnout & Suicide Report
Physicians in the U.S. are experiencing “death by 1,000 cuts,” according to the 2021 Medscape Physician Burnout & Suicide Report. Medscape polled 12,339 physicians representing over 29 specialties between late August and early November 2020 to gauge their feelings about work and life in the midst of the coronavirus pandemic. Medscape researched its first Physician Lifestyle Report in 2012. That research focused on physician “happiness” and work-life satisfaction. In 2013, the issue of burnout was called out on the cover of the report, shown here with the question, “does burnout affect lifestyle?” In 2015, the Physician Lifestyle Report was titled,
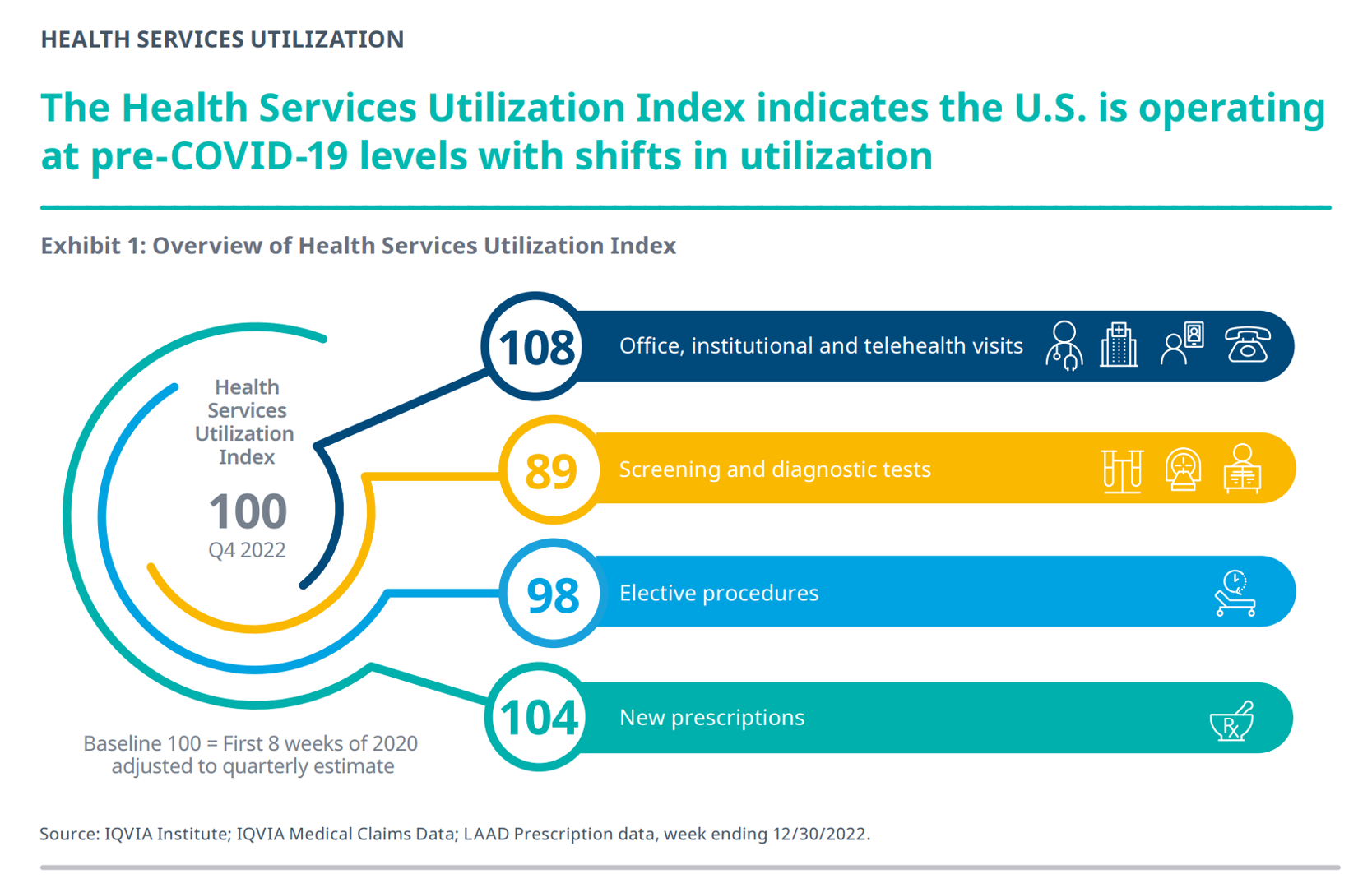
Will 2021 Be the Year of Sicker Americans? Pondering Late 2020 Data from IQVIA
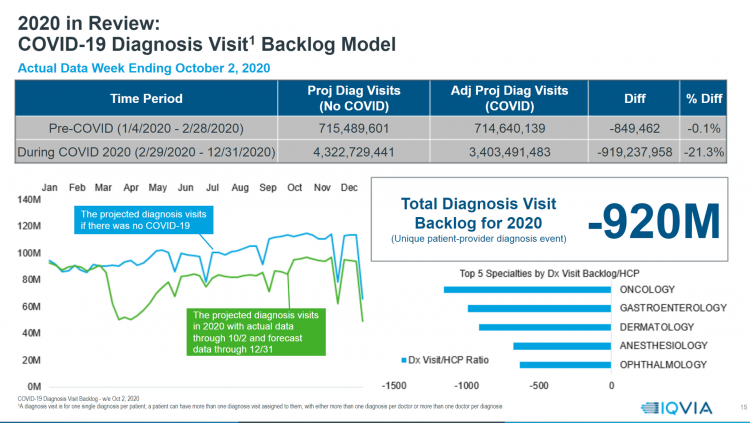
Yesterday, IQVIA presented their end-of-year data based on medical claims in the U.S. health care system tracking the ups, downs, and ups of the coronavirus in America. IQVIA has been tracking COVID-19 medical trends globally from early 2020. The plotline of patient encounters for vaccines, prescribed medicines, foregone procedures and diagnostic visits to doctors begs the question: in 2021, will Americans be “sicker,” discovering later-stage cancer diagnoses, higher levels of pain due to delayed hip procedures, and eroded quality of life due to leaky guts? Here are a few snapshots that paint a picture for greater morbidity and potentially more “excess
Behavioral Health Side-Effects in the COVID Era
“This surge of people experiencing acute behavioral health problems…has the potential to further impact the healthcare system for years to come,” a report from McKinsey expects looking at the hidden costs of COVID-19’s impact on U.S. health care. The coronavirus pandemic has taken a toll on Americans’ mental health, with anxiety and depression growing as a side-effect to worries about the virus itself, the long Great Lockdown in much of the country, and the economic recession that has particularly impacted women and people of color. I covered depression impacts due to COVID-19 here in Health Populi yesterday, and wanted to
Americans’ Sense of Well-Being Falls to Great Recession Levels, Gallup Finds
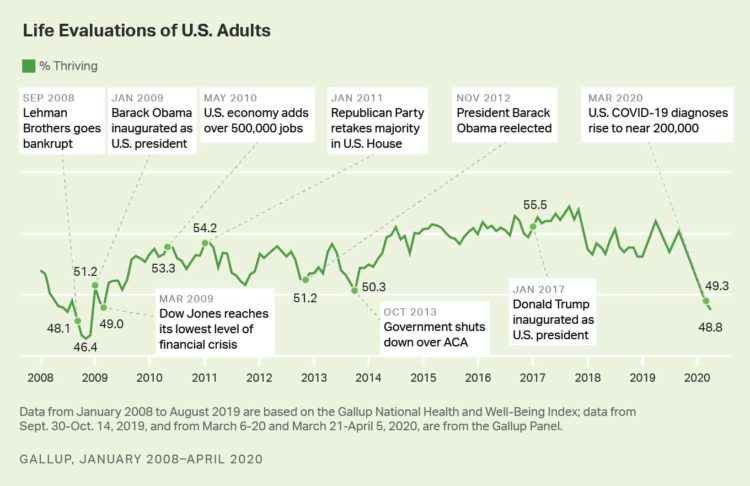
It’s déjà vu all over again for Americans’ well-being: we haven’t felt this low since the advent of the Great Recession that hit our well-well-being hard in December 2008. As COVID-19 diagnoses reached 200,000 in the U.S. in April 2020, Gallup gauged that barely 1 in 2 people felt they were thriving. In the past 12 years, the percent of Americans feeling they were thriving hit a peak in 2018, as the life evaluations line graph illustrates. Gallup polled over 20,000 U.S. adults in late March into early April 2020 to explore Americans’ self-evaluations of their well-being. FYI, Gallup asks consumers
Longevity Stalls Around the World And Wealth, More Concentrated

Two separate and new OECD reports, updating health and the global economic outlook, raise two issues that are inter-related: that gains in longevity are stalling, with chronic illnesses and mental ill health affecting more people; and, as wealth grows more concentrated among the wealthy, the economic outlook around most of the world is also slowing. First, we’ll mine the Health at a Glance 2019 annual report covering data on population health, health system performance, and medical spending across OECD countries. The first chart arrays the x-y data points of life expectancy versus health spending for each of the OECD countries
Listening to Osler Listening to the Patient – Liberating Health Care at Medecision Liberation 2019

“Listen to your patient; he is telling you the diagnosis,” Dr. William Osler is quoted to have said around the turn of the 20th century. Dr. Osler had been a strong advocate for the physician-patient conversation to inform the doctor’s diagnostic acumen and improve patient outcomes. This year is the centennial of Dr. Osler’s passing, so it’s especially timely that I introduce this post with his legendary assertion in the context of kicking off the 2019 Medecision Liberation conference. This meeting convenes the company’s clients, partners, and staff to share best practices, spark insights and learnings, and enable networking between
The Rise of Social Determinants of Health in Healthcare is Just Real Life Stuff for People, Patients, Consumers

Based on the influx of research studies and position papers on social determinants of health flowing into my email box and Google Alerts, I can say we’re past the inflection point where SDoH is embraced by hospitals, professional societies, health plans and even a couple of pioneering pharma companies. PwC published a well-researched global-reaching report this week appropriately titled, Action required: The urgency of addressing social determinants of health. The “wheel of determinants” illustrates potential partners for collaborating in communities to address SDoH factors. The collaborators include governments, health care providers, payors, life science and pharma, tech and telecomms, policy
Prelude to Health 2.0 2019: Thinking Consumers At the Center of Digital Health Transformation

“Digital transformation” is the corporate strategy flavor of the moment across industries, and the health are sector isn’t immune from the trend. As this 13th year of the annual Health 2.0 Conference kicks off this week, I’m focused on finding digital health innovations that engage people — consumers, caregivers, patients, health citizens all. This year’s conference will convene thought leaders across a range of themes, and as is the Health 2.0 modus operandi, live demo’s of new-new things. As Health 2.0 kicks off today in pre-conference sessions, there is useful context described in a new report from the American Hospital
People Want to Flourish, Not Just Live – Speaking Health Politics to Real People
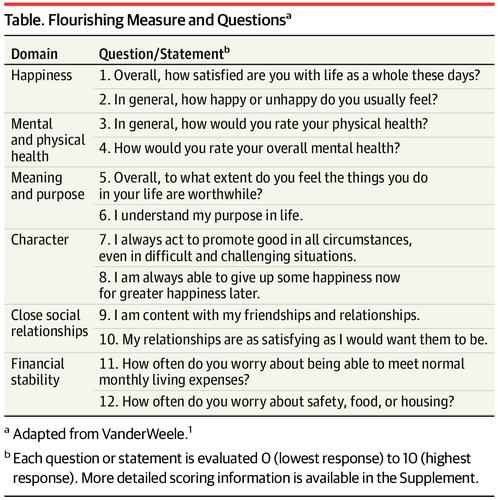
“How should we define ‘health?'” a 2011 BMJ article asked. The context for the question was that the 1948 World Health Organization definition of health — that health is, “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”– was not so useful in the 21st century. The authors, a global, multidisciplinary team from Europe, Canada and the U.S., asserted that by 2011, human health was marked less by infectious disease and more by non-communicable conditions that could be highly influenced, reversed and prevented through self-care by the individual and public health policy
How Consumers Look At Social Determinants of Health for Cancer, Diabetes and Mental Health

Enlightened health/care industry and public policy stakeholders have begun to embrace and address social determinants of health. These are the inputs that bolster health beyond health care services: they include economic stability like job security and income level (and equity), education, and access to healthy food, food security, safe neighborhoods, social support, clean environments (water and air), and in my own update on SDoH factors, access to broadband connectivity. As physician leaders in the AMA, technology advocates from AMIA, and numerous health plans focus efforts on strengthening social determinants, what do people – consumers, patients, caregivers — think about these
World Health Day 2019: Let’s Celebrate Food, Climate, Insurance Coverage and Connectivity
Today, 7 April, is World Health Day. With that in mind, I devote this post to three key social determinants of health (SDOH) that are top-of-mind for me these days: food for health, climate change, and universal health coverage. UHC happens to be WHO’s focus for World Health Day 2019. [As a bonus, I’ll add in a fourth SDOH in the Hot Points for good measure and health-making]. Why a World Health Day? you may be asking. WHO says it’s, “a chance to celebrate health and remind world leaders that everyone should be able to access the health care they need,
The Caveats for Health/Care at CES 2019

According to the Cambridge Dictionary, a “caveat” is, “a warning to consider something before doing anything more.” It is fitting that CES is held in Las Vegas, land of high risk and, with a lot of luck, reward. With that theme in mind, I depart LAS airport tonight on an aptly-named red-eye flight back home after spending an entire week here. I’m pondering not what I saw — some of which I covered daily over the past week — but what I didn’t see. Consider these the caveats for health/care at #CES2019. In no particular order… Where was the Chairman of
What #CES2019 5 Tech Trends to Watch Mean for Health/Care

As #CES2019 kicks off in Las Vegas with today’s first Media Day, the Consumer Technology Association presented its forecast on the 5 Technology Trends to Watch in 2019 — and they all play into health, wellness, and medical care. The five trends are: Artificial Intelligence on the Rise Envisioning the Smart Home of the Future Digital Health Tech Empowers Patients Esports and Sports Technology, and Smart Cities Promote Resilience. Here are how these five mega-trends can bolster our health and healthcare products and services over the next decade. AI is indeed on-the-rise in healthcare: as I have begun planning my agenda for
Disruption Is Healthcare’s New Normal
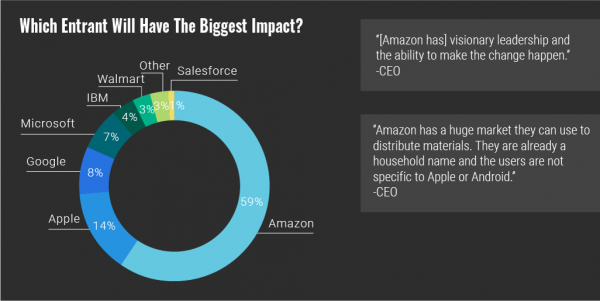
Googling the words “disruption” and “healthcare” today yielded 33.8 million responses, starting with “Riding the Disruption Wave in Healthcare” from Bain in Forbes, Accenture’s essay on “Big Bang Disruption in Healthcare,” and, “A Cry for Encouraging Disruption” in the New England Journal of Medicine Catalyst. This last article responded to the question, “Can we successfully deliver better quality care for patients at a lower cost?” asked by François de Brantes, Executive Director of the Health Care Incentives Improvement Institute. “Disruption” as a noun and an elephant in our room has been with us in healthcare since the September/October 2000 issue of
Value Comes to Healthcare: But Whose Value Is It?
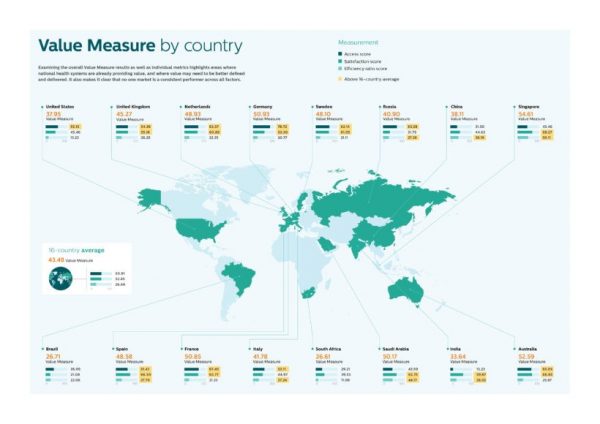
The Search for Value is the prevailing journey to a Holy Grail in healthcare these days. On that, most stakeholders working on the ground, globally. can agree. But whose value is it, anyway? Three reports published in the past few weeks give us some useful perspective on that question, woven together in today’s Health Populi blog. Let’s start with the Philips Future Health Index, which assesses value to 16 national health systems through three lenses: access, satisfaction, and efficiency. The results are shown in the map. “Value-based healthcare is contextual, geared towards providing the right care in the right place, at
Obese, Access-Challenged and Self-Rationing: America’s Health Vs Rest-of-World

The U.S. gets relatively low ROI for its relatively exorbitant spending on healthcare, noted once again in the latest Health at a Glance, the annual OECD report on member nations’ healthcare systems. The report includes U.S. country data asking, “How does the United States compare?” with its sister OECD countries. The answer is, “not well across most population health, access, and mortality measures.” For the Cliff’s Notes/Where’s Waldo top-line of the research, find the two long bars in this chart heading “south” of the OECD average, and one long blue bar going “north.” The northern climbing bar
Food as Medicine – Philips’ Take On An Apple A Day from the Rijksmuseum

What if you went to visit a Vermeer still life with fruit, vegetables, and flowers, and the only image you saw in the famous painting was the flower and an urn? What if you heard the sounds of a juicing machine whirring as you reflected on a Rembrandt? That’s exactly what happened to museum-goers visiting Amsterdam’s Rijksmuseum. These art patrons witnessed a museum guard literally pulling an apple out of a painting, to leave a barren portrait of an urn and little else. Roll over, Anthony Oberman, the artist of “Still Life with Fruit in a Terracotta Dish,” one of
Re-Imagining Healthcare – a Lesson from Von Clausewitz in the Fog of War

When you’re on the battlefield and you can’t see what lies ahead, go high, recommended General Von Clausewitz in his book, On War. I paraphrase this prescription from the good General-strategist’s book, On War — “War is the realm of uncertainty; three-quarters of the factors on which action in war is based are wrapped in a fog of greater or lesser uncertainty. A sensitive and discriminating judgment is called for; a skilled intelligence to scent out the truth.” Governor Mark Leavitt, who held the post of Secretary of Health and Human Services under President Bush, offered this advice at the recent Liberation
The Health of A Nation – Being Healthy In America Depends on Where You Live

In the US, when it comes to life and death, it’s good to live in Hawaii, Utah, Minnesota, North Dakota, and Iowa — the top five states with the greatest life expectancy and healthy life expectancy at birth in 2016. For health and longevity, sorry to see the lowest five ranked states are Washington DC which ranks last, along with Mississippi, Louisiana, South Carolina, and Alabama. This sober geography-is-health-destiny update was published this week in JAMA, The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors Among US States. The first chart illustrates states down the left
Sounds Like A John Denver Song: Virginia and Colorado Towns Rank High As Healthy Communities

If it’s true that “your ZIP code is more important than your genetic code,” you’d look for a job in 22046, buy a house there, and plant your roots. You’d find yourself in Falls Church, Virginia, named number one in the Healthiest Communities rankings of 500 U.S. towns. You can see a list of all of the communities here. The project is a collaboration between the Aetna Foundation and U.S. News & World Report, with help from the University of Missouri Center for Applied Research and Engagement Systems (CARES) and a team from the National Committee on Vital and Health
How We Spend Versus What We Get: America’s Healthcare Spending Makes for Poor Health
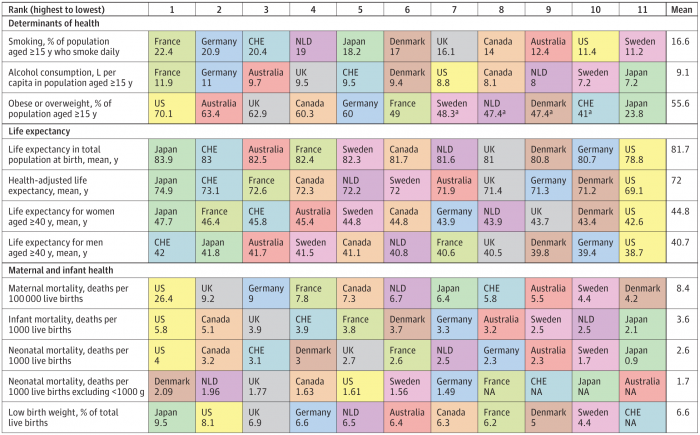
The U.S. spent nearly twice as much as other wealthy countries on healthcare, mostly due to higher prices for both labor and products (especially prescription drugs). And, America spends more on administrative costs compared to other high-income countries. What do U.S. taxpayers get in return for that spending? Lower life spans, higher maternal and infant mortality, and the highest level of obesity and overweight among our OECD peer nations. These sobering statistics were published in Health Care Spending in the United States and Other High-Income Countries this week in JAMA, the Journal of the American Medical Association. The study analyzes
What the Latest Pew Consumer Data Means for #HIMSS18
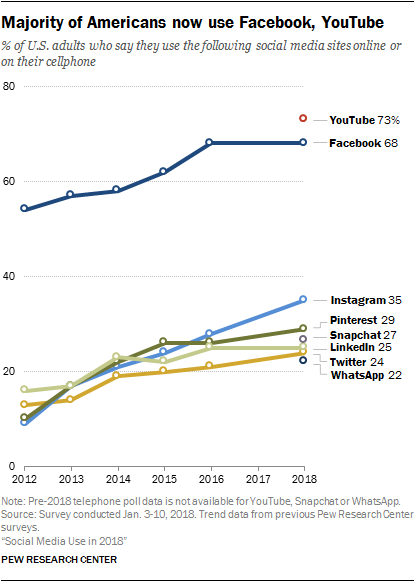
The median American uses 3 social networking platforms in 2018. Facebook is the primary platform for most Americans who use social media in 2018: two-thirds of U.S. adults use Facebook, and 3 in 4 of them check in on a daily basis. But in the past year, the percentage of people using Facebook and its corporate sister YouTube has flattened, based on the survey report, Social Media Use in 2018 from the Pew Research Center. The Pew team researched U.S. adults’ use of social media across eight popular platforms. Instagram has gained consumer favor over the past two years,
Add Behavioral Data to Social Determinants For Better Patient Understanding
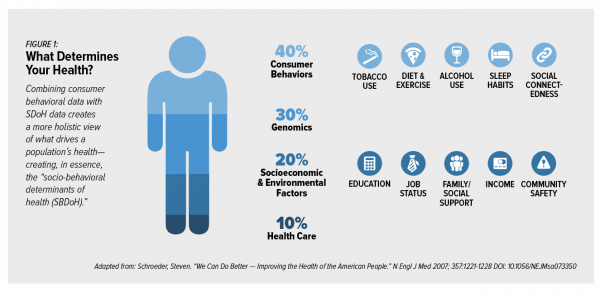
“Health agencies will have to become at least as sophisticated as other consumer/retail industries in analyzing a variety of data that helps uncover root causes of human behavior,” Gartner recommended in 2017. That’s because “health” is not all pre-determined by our parent-given genetics. Health is determined by many factors in our own hands, and in forces around us: physical environment, built environment, and public policy. These are the social determinants of health, but knowing them even for the N of 1 patient isn’t quite enough to help the healthcare industry move the needle on outcomes and costs. We need to
Heart-Love – Omron’s Holy Grail of Blood Pressure Tracking on the Wrist

It’s February 1st, which marks the first of 28 days of American Heart Month – a time to get real, embrace, learn about, and engage with heart health. Heart disease kills 610,000 people in the U.S. every year, equal to 1 in 4 deaths in America. It’s the leading cause of death for both men and women in the U.S. Knowing your blood pressure is an important step for managing the risks of heart disease. That hasn’t yet been available to those of us who quantify our steps, weight, sleep, food intake, and other health metrics. In 2017, Hugh Langley
Will Getting Bigger Make Hospitals Get Better?
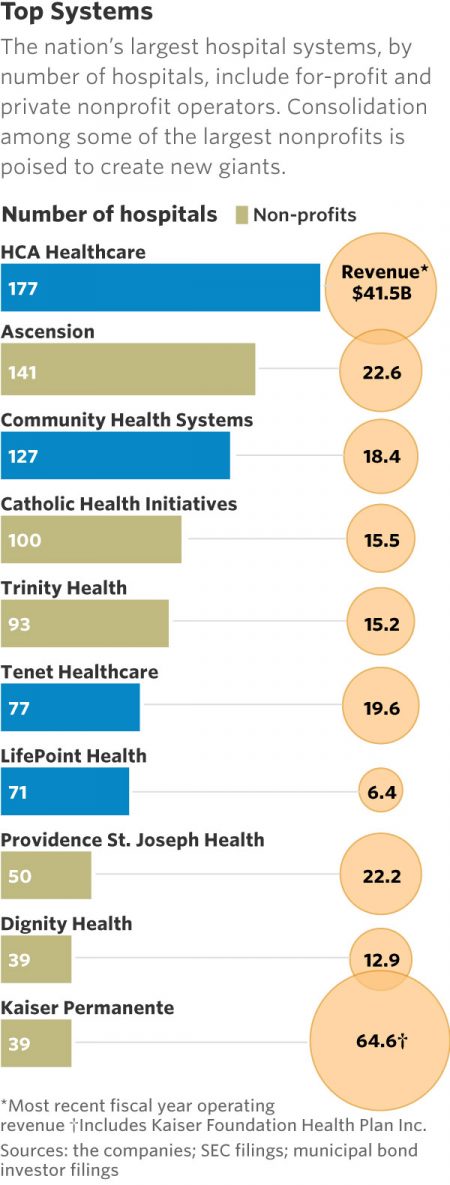
This month, two hospital mega-mergers were announced between Ascension and Providence, two of the nation’s largest hospital groups; and, between CHI and Dignity Health. In terms of size, the CHI and Dignity combination would create a larger company than McDonald’s or Macy’s in terms of projected $28 bn of revenue. (Use the chart of America’s top systems to do the math). For context, other hospital stories this week discuss in southern New Jersey. And this week, the New Jersey Hospital Association annual report called the hospital industry the “$23.4 billion economic bedrock” of the state. Add a third important item
Leveraging the Essential Data of Life: Health 2.0 – Day 1 Learnings

The future of effective and efficient healthcare will be underpinned by artful combinations of both digital technologies and “analog humans,” if the first day of the Health 2.0 Conference is a good predictor. Big thoughts about a decentralized future in healthcare kicked off Day 1 of the 11th annual Health 2.0 Conference in Santa Clara, CA. The co-founders of Health 2.0 (H20), Matthew Holt and Indu Subaiya, explained the five drivers of the tech-enabled health future. 1. The new interoperability, underpinned by FHIR standards and blockchain. “FHIR” stands for fast healthcare interoperability resources, which are informatics standards that enable data
The Mainstreaming of Wellness

“Wellness is a way to cope with the demands and rigors of new modern lifestyles,” according to Ogilvy in their latest report, The Wellness Movement Pioneers: New Global Research Findings. The report makes the case that the mass public are project-managing life adopting mental health, nutrition, physical activity and sleep to boost personal wellness. There is a big business model underneath this, which has inspired Ogilvy to start up the company’s Health & Wellness Practice. Think of this report as the group’s own business case to address the $3.7 trillion global wellness economy, illustrated by the first image. The report
Health Equity Lessons from July 23, 1967, Detroit
On July 23, 1967, I was a little girl wearing a pretty dress, attending my cousin’s wedding at a swanky hotel in mid-town Detroit. Driving home with my parents and sisters after the wedding, the radio news channel warned us of the blazing fires that were burning in a part of the city not far from where we were on a highway leading out to the suburbs. Fifty years and five days later, I am addressing the subject of health equity at a speech over breakfast at the American Hospital Association 25th Annual Health Leadership Summit today. In my talk,
Note to Mooch: The ER is Not Universal Health Care
I quote directly from the Twitter feed of Anthony Scaramucci, @scaramucci: “@dhank2525 agree. We already have Univ Health Care, we made decision long ago to treat everyone that enters an emergency room.” Mr. Scaramucci is President Trump’s Communications Chief, replacing Sean Spicer. Mr. Scaramucci is neither veteran journalist nor healthcare policy wonk. He’s a successful businessman, which I respect for his savvy and ability to build a fund, attract investors, and create a media persona which he has telegenically broadcast on CNBC and elsewhere over the past decade. He’s got a engaging public personality, and goes by the moniker, “Mooch.” But
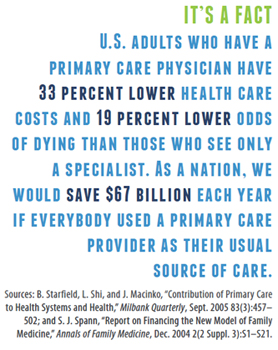
Strengthening Chronic Care Is Both Personal and Financial for the Patient
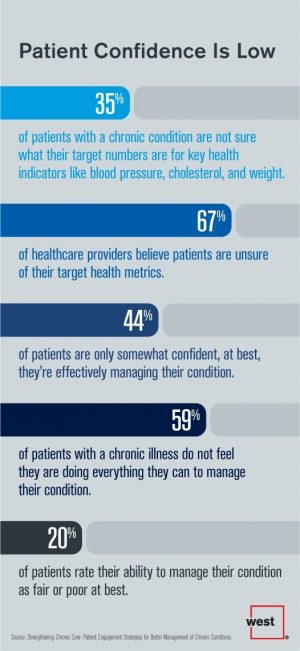
6 in 10 people diagnosed with a chronic condition do not feel they’re doing everything they can to manage their condition. At the same time, 67% of healthcare providers believe patients aren’t certain about their target health metrics. Three-quarters of physicians are only somewhat confident their patients are truly informed about their present state of health. Most people and their doctors are on the same page recognizing that patients lack confidence in managing their condition, but how to remedy this recognized challenge? The survey and report, Strengthening Chronic Care, offers some practical advice. This research was conducted by West
The Pursuit of Health Equity and the State of U.S. Health Care
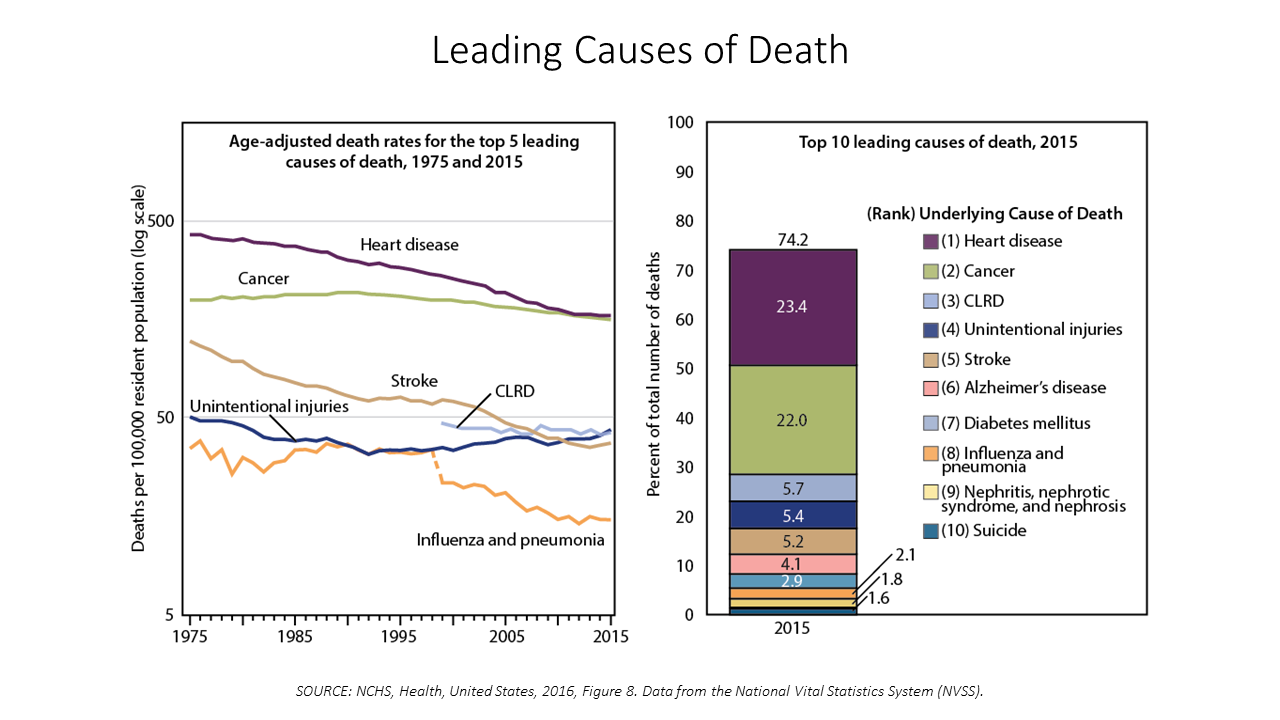
Between 2014 and 2015, death rates increased for eight of the ten leading causes; only death rates caused by cancer fell, and mortality rates for influenza and pneumonia stayed flat. The first chart paints this sobering portrait of Americans’ health outcomes, presented in the CDC’s data-rich 488-page primer, Health, United States, 2016. Think of this publication as America’s annual report on health. Every year, it is prepared and submitted to the President and Congress by the Secretary of the Department of Health and Human Services. This year’s report was delivered by DHHS Secretary Tom Price to President Trump and the
12% of Americans Have At Least 5 Chronic Conditions and Spend 41% of Healthcare Dollars
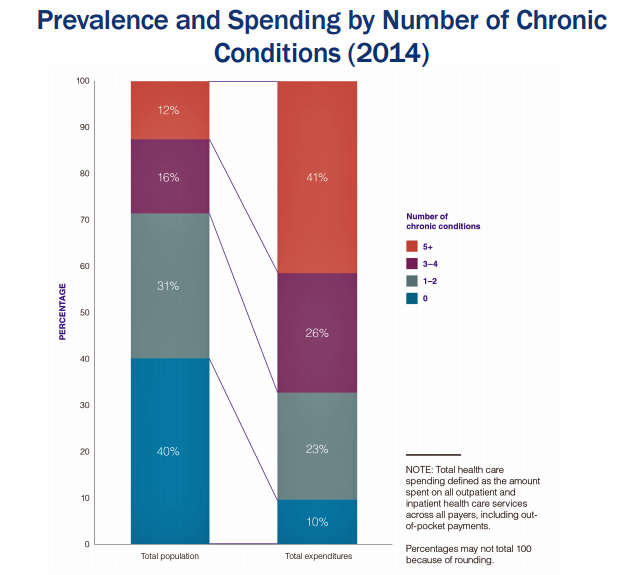
Forget about the 80/20 Rule. Welcome to the 41/12 Metric: 12% of U.S. adults account for 41% of healthcare spending in America, calculated by RAND Corporation in their new report, Multiple Chronic Conditions in the United States. RAND’s report quantifies the growing chronic care landscape in America that will be a burdensome legacy for younger Americans in terms of financial and social costs. First, a definition: RAND defines a chronic condition as a physical or mental health issue that lasts more than one year and causes functional restrictions or requires ongoing monitoring or treatment. Older adults are more likely to
The Power of Joy in Health and Medicine – Learning From Dr. Regina Benjamin

Former Surgeon General Dr. Regina Benjamin was the first person who quoted to me, “Health isn’t in the doctor’s office. It’s where people live, work, play and pray,” imparting that transformational mantra to me in her 2011 interview with the Los Angeles Times. I wrote about that lightbulb moment here in Health Populi. Dr. Benjamin was the 18th Surgeon General, appointed by President Obama in 2009. As “America’s Doctor,” she served a four-year term, her mission focused on health disparities, prevention, rual health, and children’s health. Today, Dr. Benjamin wears many hats: she’s the Times Picayune/NOLA.com professor of medicine at
Telehealth and Virtual Healthcare Are Mainstreaming
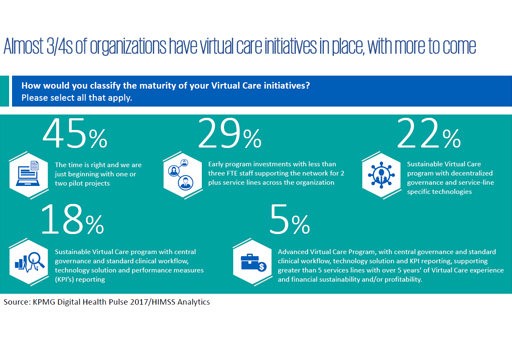
As the annual meeting of the American Telemedicine Association convenes this week in Orlando, there’s a lot of telehealth news to curate. The topline of it all: virtual healthcare is mainstreaming, with more providers, payors, and patients aligning in support of virtual health care delivery. Three-quarters of providers have some form of basic telemedicine or telehealth in place. One-third of healthcare providers use some flavor of virtual care technology in their workflow, according to research from KPMG and HIMSS Analytics summarized in the first graphic. KPMG sees virtual care options — remote patient monitoring, enhanced portals, and web interactions for patient-provider
Health Inequity in the United States – A View From Across the Pond
The statistics on the health of people living in America illustrate a divide between have’s and have-not’s. Average life expectancy is lower in the US compared with other wealthy nations: the wealthiest Americans live 10 to 15 years longer than the poorest, according to a landmark article in JAMA from 2016 studying the relationship between income inequality and mortality. See the first chart: this illustrates that people living in the US whose income reaches the top 95th percentile far outlive folks in the bottom 5th percentile of income. I find myself in London, England, this week, across the Pond (that is,
Connecting the Dots Between Population Health and the Local Economy
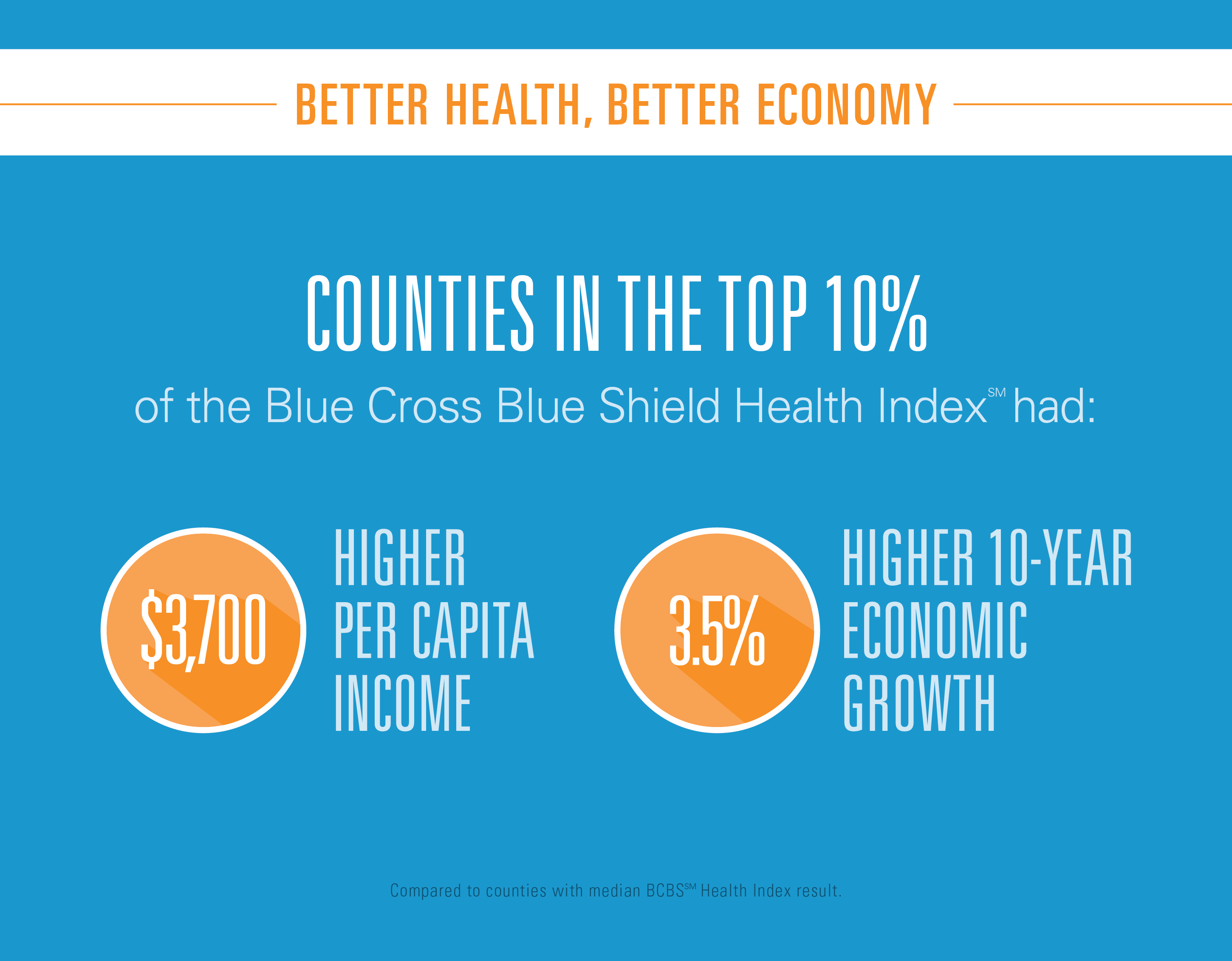
U.S. counties with better health have better performing economies. There’s a direct link between healthy people and a healthy economy, where healthier regions enjoy lower unemployment and higher incomes, according to the Blue Cross Blue Shield Health Index. When compared to counties with a median BCBS Health Index score, counties within the top 10 percent had: A per capita income that’s $3,700 higher than the median 10-year economic growth that’s 3.5% higher An unemployment rate half a point lower. The Blue Cross Blue Shield Association (BCBSA) worked with Moody’s Analytics (part of the Moody’s financial services company) on this second edition of this
A New Risk Factor For Mental Health: Climate Change
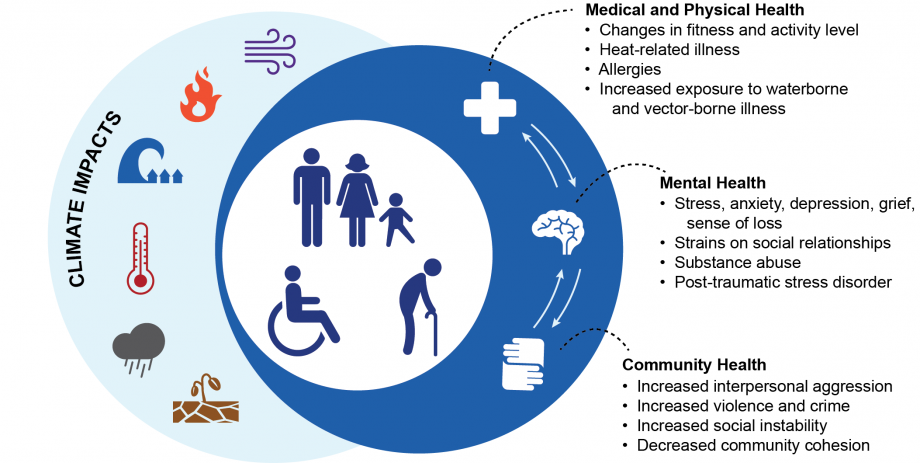
We make our health across many dimensions: via nutrition, safe physical/built environments, financial wellness, education, and the environment among them. In this last category, the environment, new research finds that climate change has a significant impact on health. The report, Mental Health and Our Changing Climate: Impacts, Implications, and Guidance, was sponsored by the American Psychological Association in conjunction with Climate for Health and ecoAmerica. “Climate change-induced severe weather and other natural disasters have the most immediate effects on mental health in the form of the trauma and shock due to personal injuries, loss of a loved one, damage to
States That Expanded Medicaid Improved Healthcare Access & Patient Outcomes
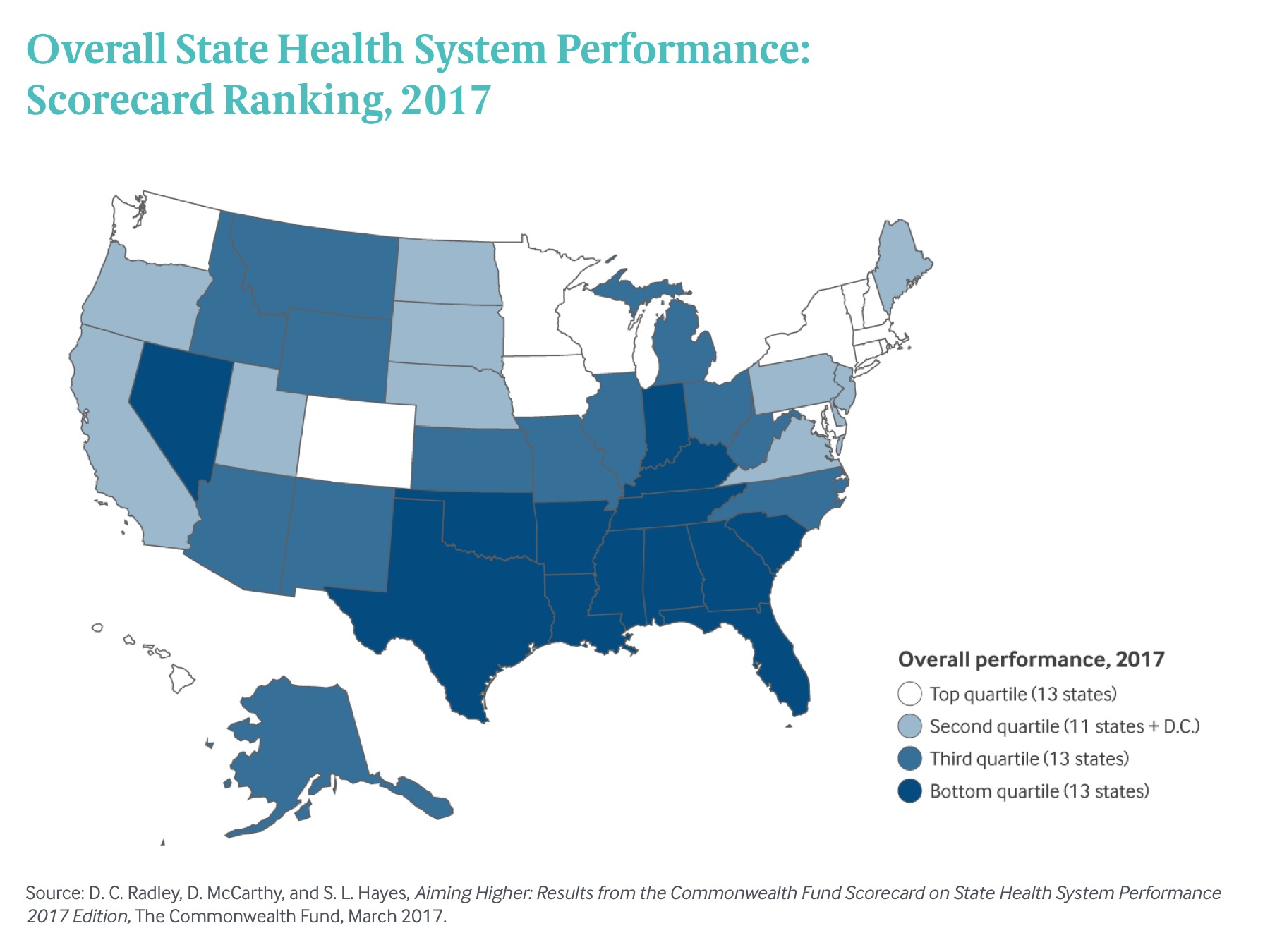
States that expanded Medicaid since the start of the Affordable Care Act made greater health system access improvements than those States that did not expand Medicaid, according to Aiming Higher: Results from the Commonwealth Fund Scorecard on State Health System Performance. There’s good news and bad news in this report: on the upside, nearly all states saw health improvements between 2013 and 2015, and in particular, for treatment quality and patient safety. Patient re-admissions to hospitals also fell in many states. But on the downside, premature deaths increased in nearly two-thirds of states, a reversal in the (improving) national mortality
Your Zip Code Is Your Wellness Address

Geography is destiny, Napoleon is thought to have first said. More recently, the brilliant physician Dr. Abraham Verghese has spoken about “geography as destiny” in his speeches, such as “Two Souls Intertwined,” The Tanner Lecture he delivered at the University of Utah in 2012. Geography is destiny for all of us when it comes to our health and well-being, once again proven by Gallup-Healthways in The State of American Well-Being 2016 Community Well-Being Rankings. The darkest blue circles in the U.S. map indicate the metro areas in the highest-quintile of well-being. The index of well-being is based on five metrics, of consumer self-ranking
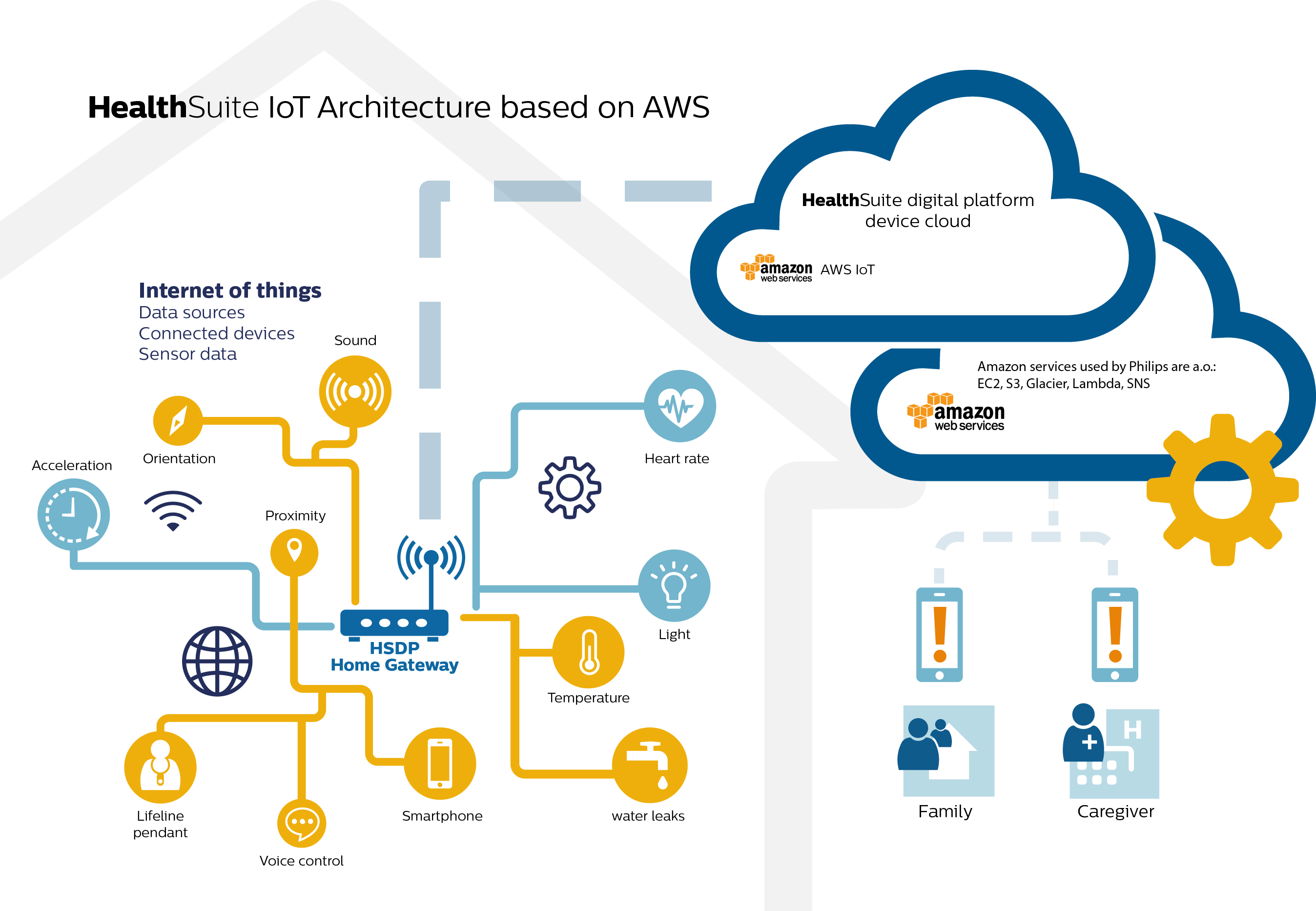
How the Internet of Things Will Support Health at Home
There’s a concept in healthcare called the patient-centered medical home (PCMH). In 2007, the primary care providers’ (PCPs) medical societies (e.g., American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, and the American Osteopathic Association) envisioned the PCMH to be the first touch-point for a health consumer with the health system. As such, the PCMH would be the “medical home” for a consumer, directed by a personal physician who takes responsibility for the ongoing care of patients. For some time, I’ve been evangelizing about our actual homes as our medical (or better put, health) homes. Who better to
Images of Health, Vitality and Life at #HIMSS17

The plane has left the Orlando airport, and I’m looking back at the past week at the 2017 annual meeting of HIMSS, the annual health IT conference that has been my pleasure and (foot) pain to attend for the past two+ decades (for real). Walking the exhibition floor, I encountered some new flavors of imaging that went way beyond bits and bytes, data and technology. These images spoke to me of health, vitality, and life. I’m sharing them with you here, with no intention of selling you company products or services but simply sharing some images that speak to these
From EHRecords to EHDelivery: Talking With Dr. Roy Schoenberg of American Well

Telehealth has come of age at HIMSS in 2017. No longer is the concept relegated to footnote or edge-booth status on the conference floor. Instead, telehealth, broadly defined, is now a mainstream concept embraced by healthcare providers, payors and, increasingly, consumers. I spent time brainstorming telehealth with one of the pioneers of modern telehealth in the U.S., Dr. Roy Schoenberg, who co-founded American Well with his brother Ido Schoenberg, in 2007. As such, the company is among the most mature telehealth entities operating in America, delivering live video health visits to millions of health consumers through the American Well telehealth
Healthcare and the Autonomous Car: Setting the Stage for HIMSS17

The autonomous car is a metaphor for healthcare: that’s how my first interview kicking off the HIMSS marathon began. The annual 2017 HIMSS conference isn’t your father’s or mother’s HIMSS of ten years ago, or even the HIMSS of 2010 — the year that financial incentives for EHR adoption began to stream from the HITECH Act of 2009, motivating thousands of healthcare providers to acquire and meaningfully use digital health records systems. Then, the HIMSS conference floor was abuzz with EHR frenzy. This week, over 43,000 people working at the intersection of healthcare and technology have converged in Orlando, Florida, for
Digital Technology Is A Bridge To Healthcare Consumers: A HIMSS Preface

“Digital technology can provide a bridge to the healthcare system via sensors, tools, and trackers for people who are living their lives each day,” I explained to the social media team at Philips, which is morphing as an organization to being all digital health, all-the-time. (Here’s what I learned about Philips and digital health in January 2017 after meeting with Jeroen Tas at the CES in Vegas). Here’s the larger discussion, shared with several of my fellow members of the HIMSS Social Media Ambassador family. I’ll be meeting with Philips’ leadership at HIMSS, the annual health IT conference that
The Health Disparity of Information Access
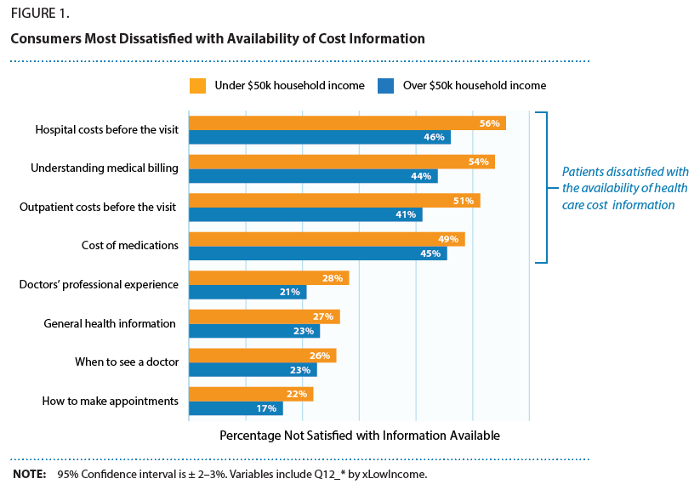
Among many health disparities which mar healthcare quality in the United States, there’s another one to add to the list: health and healthcare information access. Access to health care is underpinned in large part on a health consumer’s access to information about available health care services, their location, price, and if the patient is very fortunate to glean, quality. As people take on more responsibility for managing their health care utilization and financing in America, their access to information that is easy-to-find, clear, comprehensive and current is critical to personal and public health outcomes. But consumers are dissatisfied with the
More Consumers Use Retail Health Clinics for Healthcare Management, Harris Finds
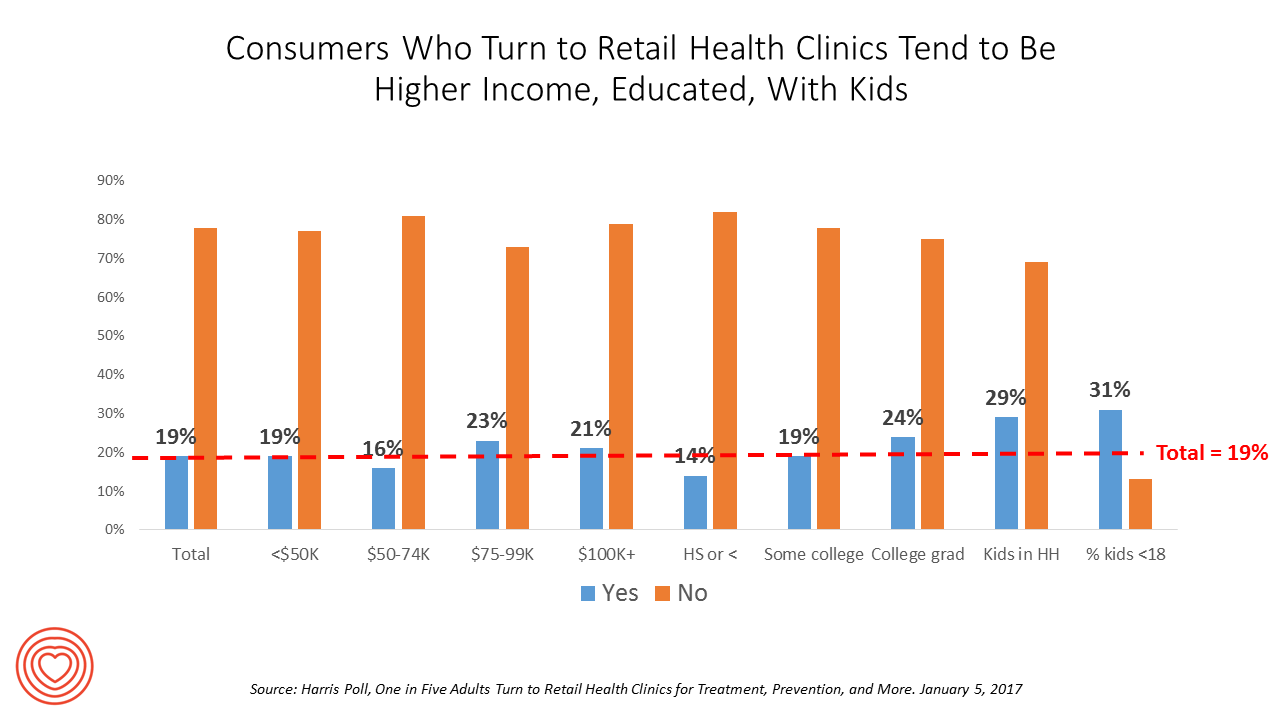
1 in 5 U.S. adults used a retail clinic in 2016. Increasingly, health consumers seek care from retail clinics for more complex healthcare services beyond flu shots and pre-school exams, according to the Harris Poll’s survey, One in Five Adults Turn to Retail Health Clinics for Treatment, Prevention, and More, published January 5, 2017. Additional points the poll revealed are worth attention for public health policy purposes: Twice as many people who identify as LGBT turn to retail clinics than others (35% vs. 18%) Older people frequent retail clinics for flu vaccines more than younger people do More younger men
Health/Care Data Ecosystems E-merge at CES 2017

Digital health innovations were fast-proliferating at CES 2017. The bad news is there are so many of them, it’s dizzying and fragmented. The good news is that there are emerging health data ecosystems that will streamline consumers’ user experience so that people can derive knowledge, actionable advice and value out of using these tools. Walking miles of aisles in the Sands Convention Center in the first week of January 2017 can be a dizzying prospect, with hype and best-faces-forward in every single exhibitor at the show. In the health segment at CES, there’s a long list of digital tools to
Dying Younger in America
For the first time since 1993, expanding life expectancy in the United States has reversed, based on the latest report from the Centers for Disease Control, Mortality in the United States, 2015. “The last time U.S. life expectancy at birth declined was in 1993, when it dropped from 75.6 to 75.4, according to World Bank data,” as quoted in the Washington Post. Life expectancy at birth in 2015 was 78.8 years, a slight fall from 2014 at 78.9 years. The larger decline fell among men, from 76.5 to 76.3 years. For women, life expectancy at birth in 2015 was 81.2,
1 in 3 Americans Still Self-Rations Healthcare
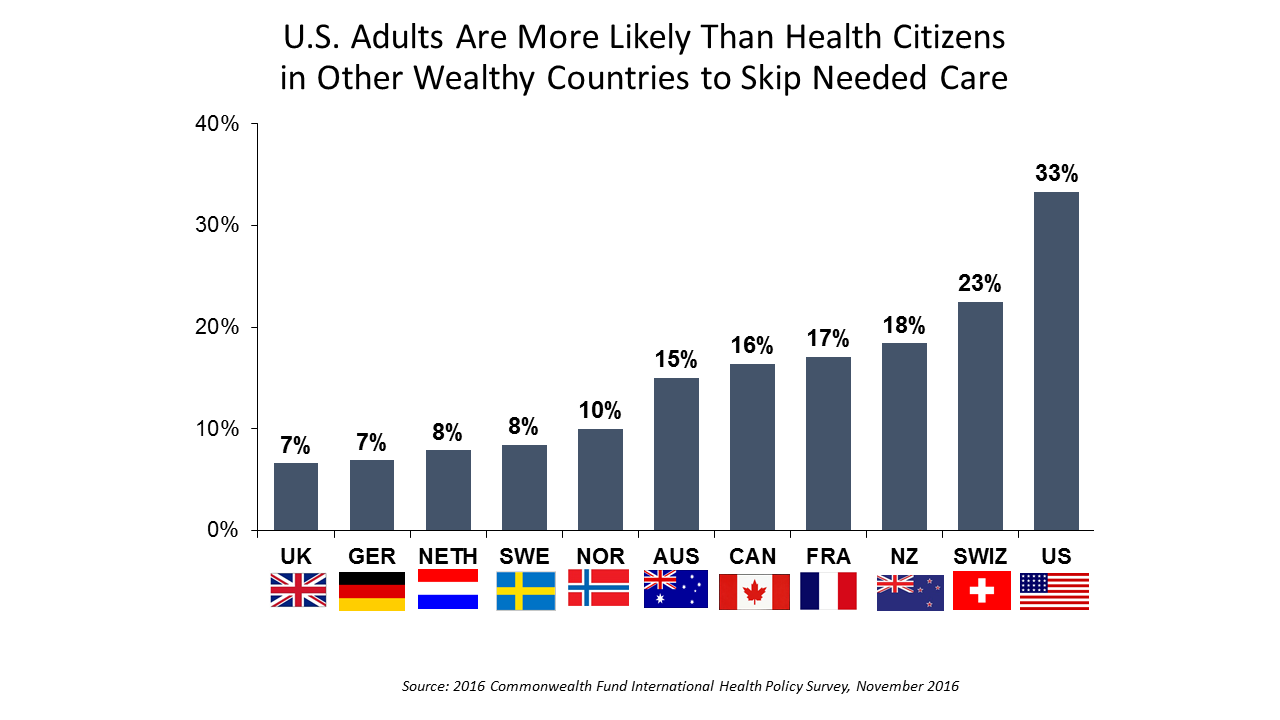
People in the U.S. are much more likely to go without health care they need compared with health citizens in 10 other wealthy countries, according to the Commonwealth Fund’s 2016 international survey. One-third of Americans did not seek care due to costs, including going without recommended care, failing to fill a prescription drug, and/or not seeing a doctor when sick. While this self-rationing proportion of Americans dropped from 37% in 2013, the U.S. still ranks #1 in foregoing necessary healthcare due to cost. “In comparison to adults in the other 10 countries, adult sin the U.S. are sicker and more




 I'm gobsmackingly happy to see my research cited in a new, landmark book from the National Academy of Medicine on
I'm gobsmackingly happy to see my research cited in a new, landmark book from the National Academy of Medicine on 
 Grateful to Gregg Malkary for inviting me to join his podcast
Grateful to Gregg Malkary for inviting me to join his podcast