Health Care Nation – How to Inspire a Rosa Parks Moment for Healthcare in America?
Tom Lawry may be best-known as a leading voice on AI in health care; after all, he’s written two very well-selling books on the topic, speaks all over the world on the subject, and in his most recent company-based gig helped lead Microsoft’s efforts in AI in health care and life sciences. When his publisher asked him to write a third book on AI in health care – still a hot topic in publishing – Tom said he’d rather turn to a subject long on his mind: the state of health care in America and how to change the conversation
The Rough Guide to Health/Care Consumers in 2025: The 2025 Health Populi TrendCast
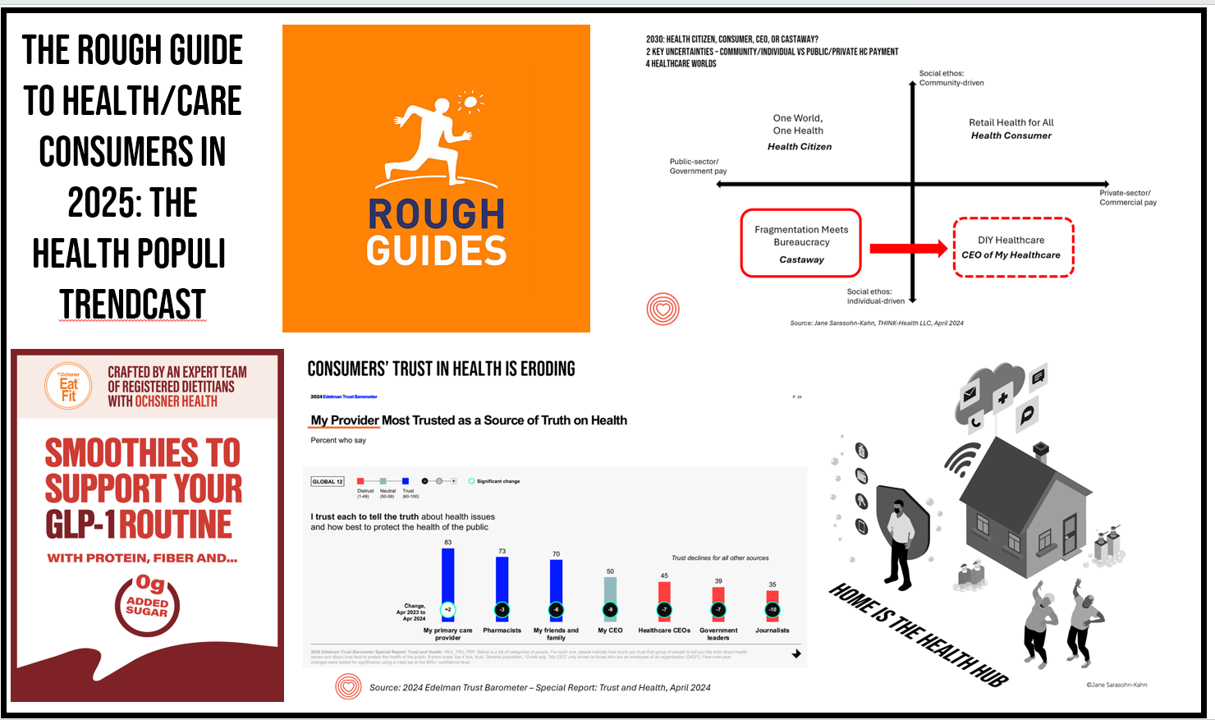
At this year-end time each year, my gift to Health Populi readers is an annual “TrendCast,” weaving together key data and stories at the convergence of people, health care, and technology with a look into the next 1-3 years. If you don’t know my work and “me,” my lens is through health economics broadly defined: I use a slash mark between “health” and “care” because of this orientation, which goes well beyond traditional measurement of how health care spending is included in a nation’s gross domestic product (GDP); I consider health across the many dimensions important to people, addressing physical,
Americans Want More Health Care Issues Baked into the 2024 Elections – Gallup
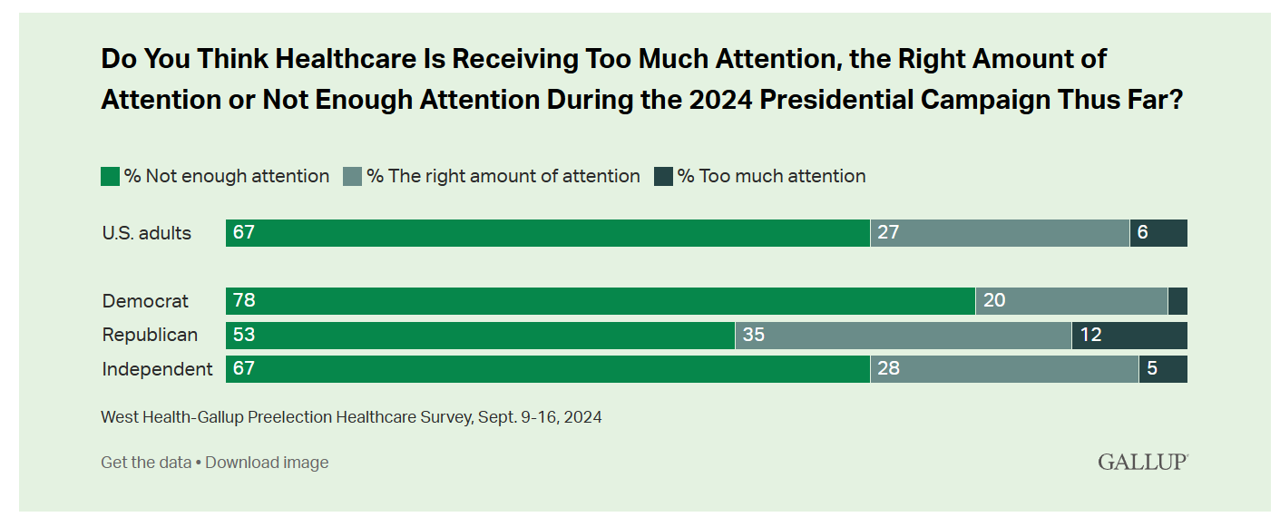
Beyond women’s health and abortion politics, most Americans are looking for more health care baked into the 2024 Elections, based on a new poll from Gallup in collaboration with West Health. Two in three U.S. adults thought health care was not receiving enough attention during the 2024 Presidential campaign as of September 2024. This is a majority shared opinion for voters across the three party IDs in the U.S., shown in the first bar graph. The research polled 3,660 U.S. adults in September, about two-thirds before the presidential debate held September 10, and about one-third
Leveraging Trust, Showing Humility: How Health Care Organizations Can Serve Consumers – A New Read from McKinsey
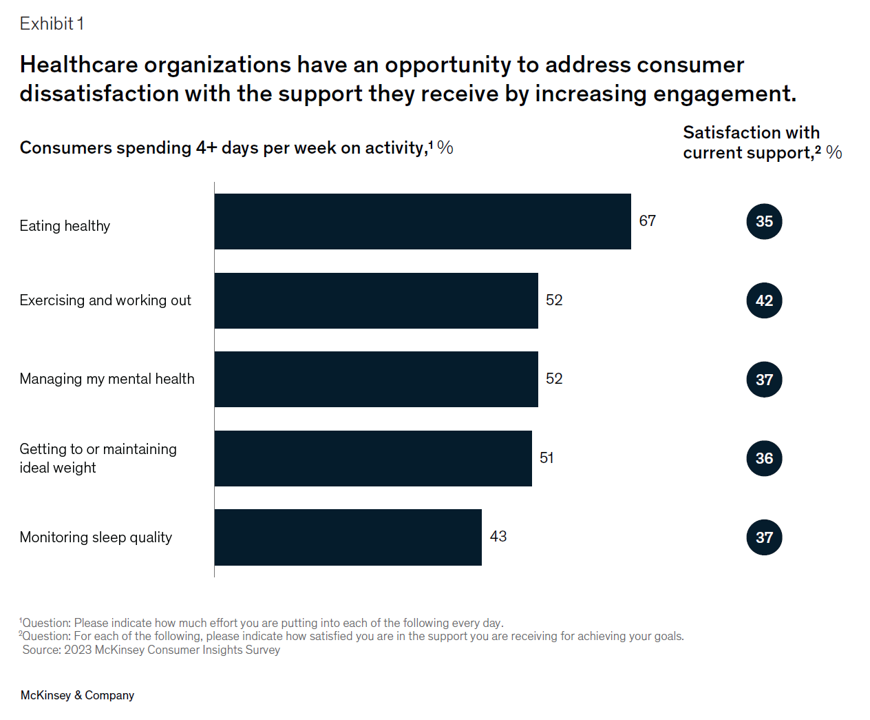
Three trends underpin health consumers’ evolving demands for service: spending more but getting less satisfaction and innovation; trusting health care with data but underwhelmed by the use of that personal information; and, growing “shopping” behavior seeking quality, availability, proximity, cost, and options across channels for health care. That’s the current read from McKinsey & Company’s team noting that Consumers rule: Driving healthcare growth with a consumer-led strategy. In this health consumer update, McKinsey spoke with three consumer marketing experts from other industries to learn best practices on how best to “be there”
Clinician Burnout – Lessons from BDO’s Clinician Experience Survey for Patient Experience and Primary Care
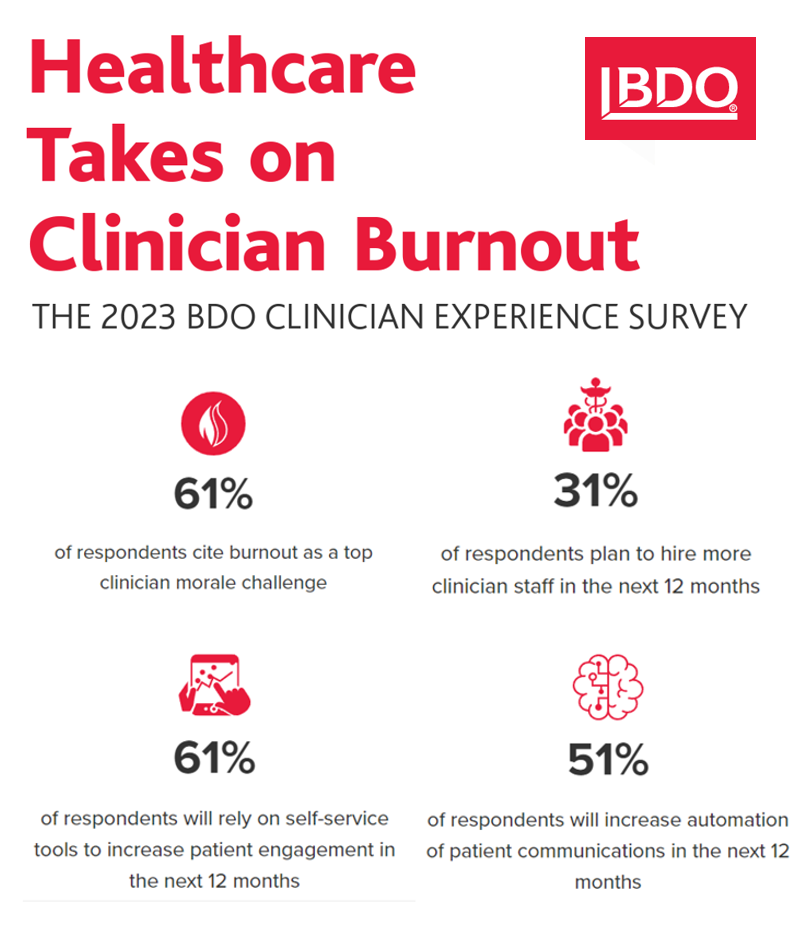
Clinicians’ feeling burnout is the top morale challenge facing U.S. doctors, driven by turnover and understaffing, compassion fatigue, and challenges using digital tools — think EHRs. The 2023 BDO Clinician Experience Survey “takes on” clinician burnout, connecting the strategic dots between the clinician experience and the patient experience. BDO surveyed 153 clinician leaders in June and July 2023; one-half of the clinicians were executive leaders, and one-fourth were each direct clinician providers and clinician directors. Roles reached into the C-suite (one-third), and other levels in their organizations.
Three More Signposts on the Road to Retail Health – Weight Loss Drugs, OTC Birth Control and Fashion-Meets-the-Flu
We continue to track to evolving, expanding landscape of retail health — which we see as the expanding ecosystem of health/care accessible to people-as-health consumers. This week, three intriguing examples are resonating with us: The ever-evolving weight-loss industry FDA favors OTC use for Perrigo’s Opill daily oral contraceptive birth control pill The convergence of fashion and health — specifically, how an over-the-counter medicine converges with clothing that helps us feel better. Let’s start with weight-loss, as several aspects of health/care come together in the consumer’s retail health sandbox. Dr. Eric Topol
The Top 10 Patient Safety Concerns for 2023 Are About Social, Mental and Behavioral Health
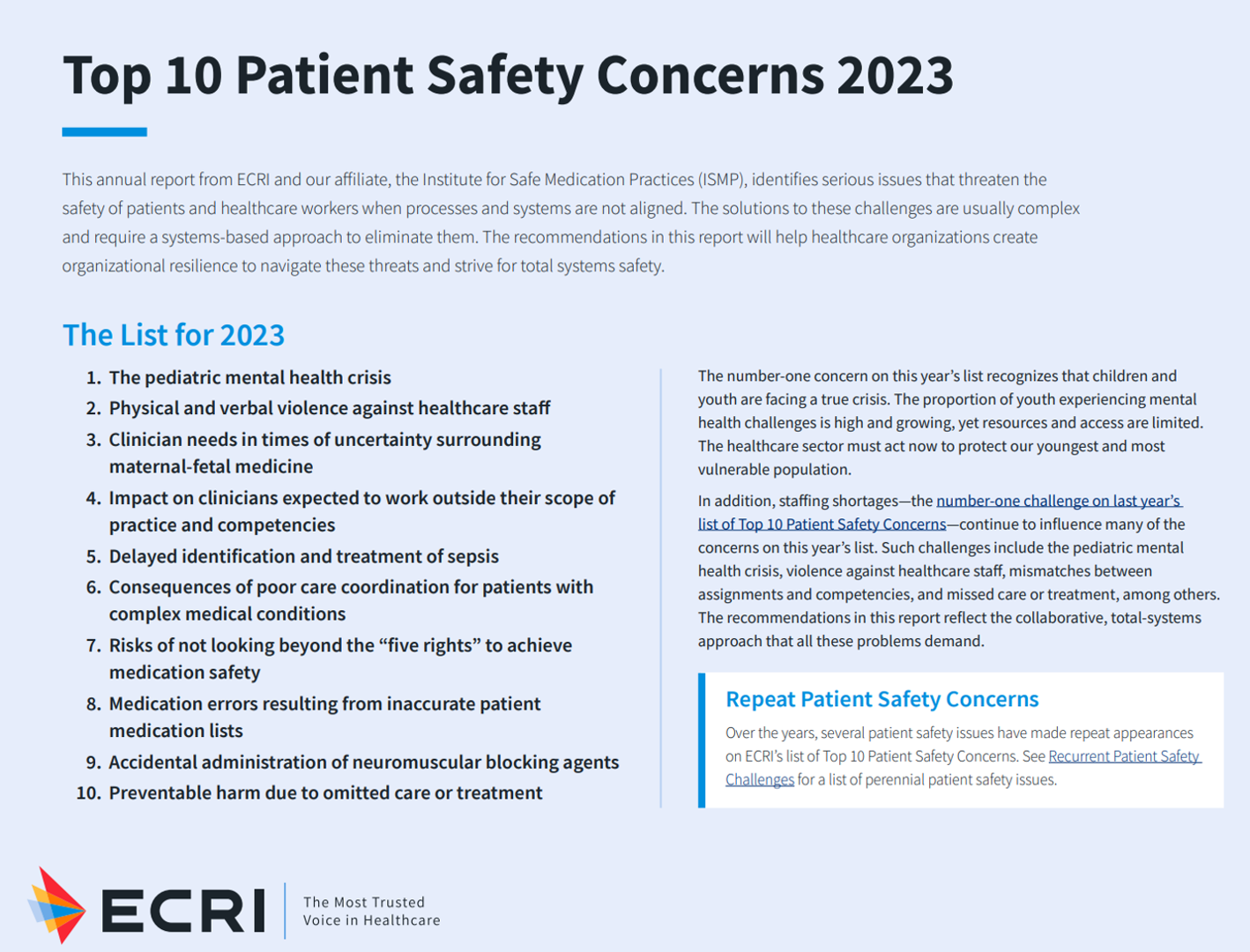
Ten years ago, ECRI named the top 10 health technology hazards for 2013: they were alarm hazards, medication administrative errors using infusion pumps, unnecessary exposure and radiation burns from diagnostic radiology procedures, patient/data mismatches in EHRs and other HIT systems, interoperability failures with medical devices and health IT systems, and five other tech-related hazards. In 2014, ECRI pivoted the title of this annual report to “patient safety concerns,” a nuance away from health technology. Fast forward to 2023 and ECRI’s latest take on the Top 10 Patient Safety Concerns 2023. While technology is embedded in this list, the headlines have more
The Patient As the Payer: Self-Pay, Bad Debt, and the Erosion of Hospital Finances
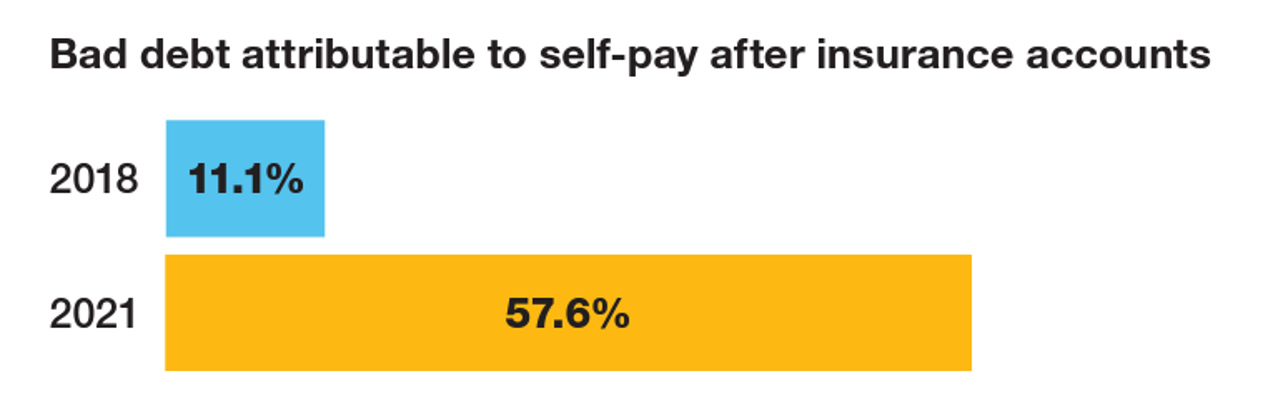
“The odds are against hospitals collecting patient balances greater than $7,500,” the report analyzing Hospital collection rates for self-pay patient accounts from Crowe concludes. Crowe benchmarked data from 1,600 hospitals and over 100,00 physicians in the U.S. to reveal trends on health care providers’ ability to collect patient service revenue. And bad debt — write-offs that come out of uncollected patient bill balances after “significant collection efforts” by hospitals and doctors — is challenging their already-thin or negative financial margins. The first chart quantifies that bad debt attributable to patients’ self-pay payments
Doximity Study Finds Telehealth Is Health for Every Day Care
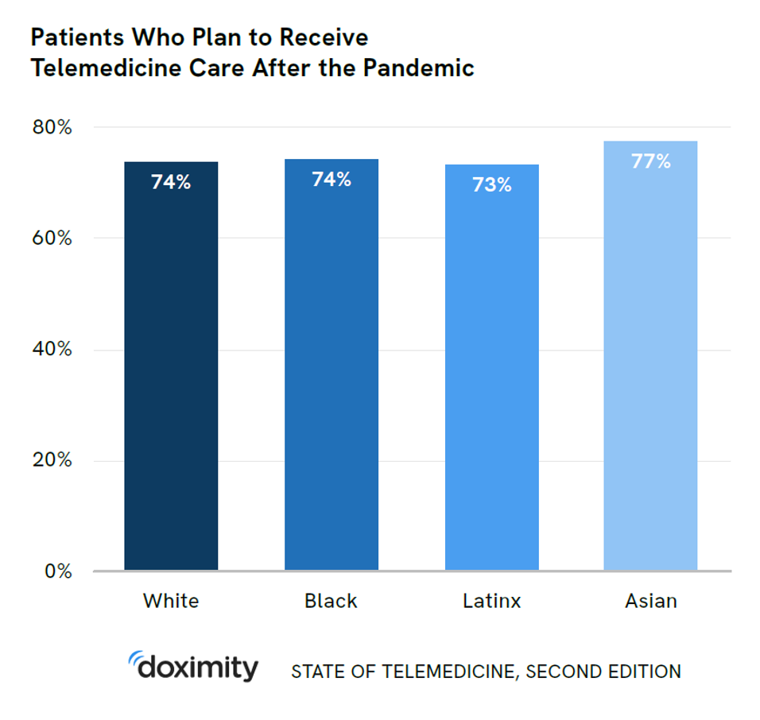
There’s more evidence that doctors and patients, both, want to use telehealth after the COVID-19 pandemic fades. Doximity’s second report on telemedicine explores both physicians’ and patients’ views on virtual care, finding most doctors and health consumers on the same page of virtual care adoption. For the physicians’ profile, Doximity examined 180,000 doctors’ who billed Medicare for telemedicine claims between January 2020 and June 2021. Telemedicine use did not vary much across physician age groups. Doctors in specialties that manage chronic illnesses were more likely to use telehealth: endocrinology (think: diabetes), gastroenterology, rheumatology, urology, nephrology, cardiology, ENT, neurology, allergy, and
What Health Care Can Learn from Chick-fil-A, Clorox, and Chewy – Liberating Health

When we think about “3 C’s” for health care experience leadership, we might turn to Cleveland Clinic, Cigna, and CVS/health. In my latest post for the Medecision Liberation site, I point to a new trio of “C’s” to inform and inspire our patient/consumer/caregiver experience designs: Chick-fil-A, Clorox, and Chewy. Why these three? I explain, “Whether you share enthusiasm for these brands or not, news outlets and industry observers have noted these three organizations have weathered the pandemic well when it comes to improving the consumer experience and increasing customer engagement and satisfaction.” What health care can learn: These organizations streamlined
Telehealth Use Among Older Americans: Growing Interest, Remaining Concerns
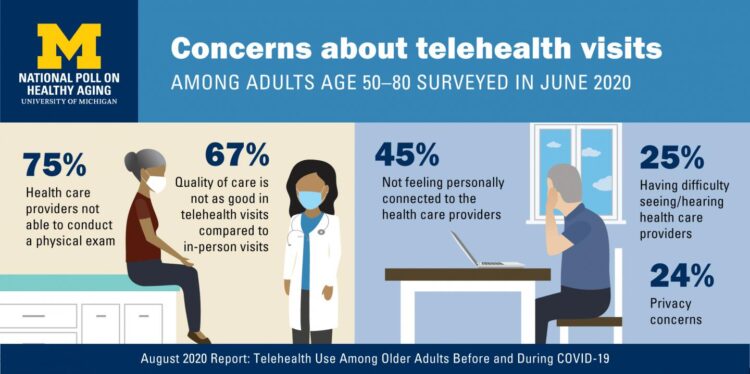
In the Fear of Going Out Era spawned by the COVID-19 pandemic, many patients were loath to go to the doctor’s office for medical care, and even less keen on entering a hospital clinic’s doors. This drove health consumers to virtual care platforms in the first months of the public health crisis — including lots of older people who had never used telemedicine or even a mobile health app. In the August 2020 National Poll on Heathy Aging, the University of Michigan research team found a 26% increase in telehealth visits from 2019 to 2020, March to June 2020 year-over-year.
Trust Is the Currency for Consumer Health Engagement – A Bottom-Line at CES 2020
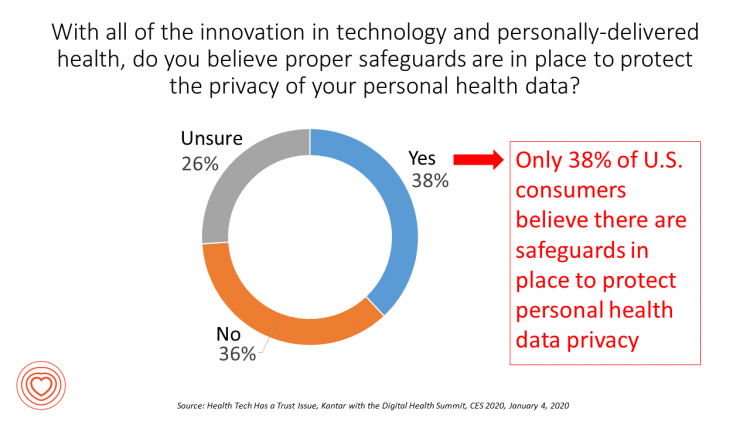
There’s less talk about Bitcoin and cryptocurrency at #CES2020. The most important currency under discussion is Trust. We have begun a consumer electronics migration from the past decade of the Internet of Things to this next decade of the Intelligence of Things. The different “I’s” signal the transition from devices that have connected to the Internet and generated data from our everyday lives, to the next ten years of gathering that data, mashing it up for meaning, and feeding back intelligence to users in the form of advising, coaching, nudging — with potentially powerful feedback loops for health, wellness and
A Portrait of the Health Consumer as Confused, Cost-Challenged, and Out of Control

Patients in the U.S. are confused, cost-challenged and lacking control, according to The Consumer Healthcare Paradox from Maestro Health, an employee health and benefits company. Data illustrating that “paradox” is shown in the second chart: while 78% percent of patients told Maestro Health their health care experience is positive, 69% feel they lack control over their patient journey. Quality health care in America is too expensive, 79% of consumers said. Furthermore, one in two U.S. patients had received a medical bill that was higher than they anticipated it would be. Finally, one in two U.S. patients said the quality of
Patients, Health Consumers, People, Citizens: Who Are We In America?

“Patients as Consumers” is the theme of the Health Affairs issue for March 2019. Research published in this trustworthy health policy publication covers a wide range of perspectives, including the promise of patients’ engagement with data to drive health outcomes, citizen science and participatory research where patients crowdsource cures, the results of financial incentives in value-based plans to drive health care “shopping” and decision making, and ultimately, whether the concept of patients-as-consumers is useful or even appropriate. Health care consumerism is a central focus in my work, and so it’s no surprise that I’ve consumed every bit of this publication. [In
How MedModular Fits Into the New Lower-Cost, High-Quality, Consumer-Enchanted Healthcare World

In American health economics, there’s a demand side and a supply side. On the demand side, we’ve done a poor job trying to nudge patients and consumers toward rational economic decision making, lacking transparency, information symmetry, and basic health literacy. On the supply side, we’ve engaged in a medical arms race allocating capital resources to shinier and shinier new things, often without cost-benefit rationale or clinical evidence. On that supply side, though, I met up with an innovation that can help to bend the capital cost curve of how we envision and build new hospitals and clinics. This week, I
Value Comes to Healthcare: But Whose Value Is It?
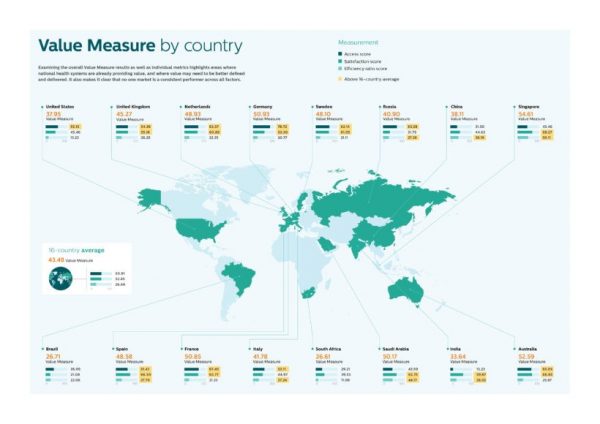
The Search for Value is the prevailing journey to a Holy Grail in healthcare these days. On that, most stakeholders working on the ground, globally. can agree. But whose value is it, anyway? Three reports published in the past few weeks give us some useful perspective on that question, woven together in today’s Health Populi blog. Let’s start with the Philips Future Health Index, which assesses value to 16 national health systems through three lenses: access, satisfaction, and efficiency. The results are shown in the map. “Value-based healthcare is contextual, geared towards providing the right care in the right place, at





 I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider
I love sharing perspectives on what's shaping the future of health care, and appreciate the opportunity to be collaborating once again with Duke Corporate Education and a global client on 6th May. We'll be addressing some key pillars to consider in scenario planning such as growing consumerism in health care, technology (from AI to telehealth), climate change, and trust -- the key enabler for health engagement or dis-engagement and mis-information. I'm grateful to be affiliated with the corporate education provider  Thank you FeedSpot for
Thank you FeedSpot for